|
Back to 2016 Annual Symposium Abstacts
Trends in incidence and indications for primary amputation for peripheral arterial disease in a population based study
Animesh Rathore, MBBS, Manju Kalra, MBBS, Thomas Bower, MD, Audra A. Duncan, MD, Gustavo S. Oderich, MD, Mark D. Fleming, MD, Randall R. De Martino, MS, William S. Harmsen, MS, Courtney Heins, BS, Peter Gloviczki, MD.
Mayo Clinic, Rochester, MN, USA.
Objective: The aim of this study was to evaluate trends in incidence and indications for primary amputation (PA) without prior revascularization in patients with peripheral arterial disease (PAD) between 1990 and 2009 in a defined population.
Methods:
All procedures (revascularization and amputation) performed for PAD were identified by ICD9/CPT codes from a population based database for residents of a single county. Primary amputations (PA) without prior revascularization were selected for inclusion in the study. Patient demographics and indications for PA were elucidated from the medical record. Non-PAD related amputations were excluded. Incidence rates were calculated for 5-year periods. Poisson regression models adjusted for age and sex were used to test secular trends in 5-year incidence rates.
Results:
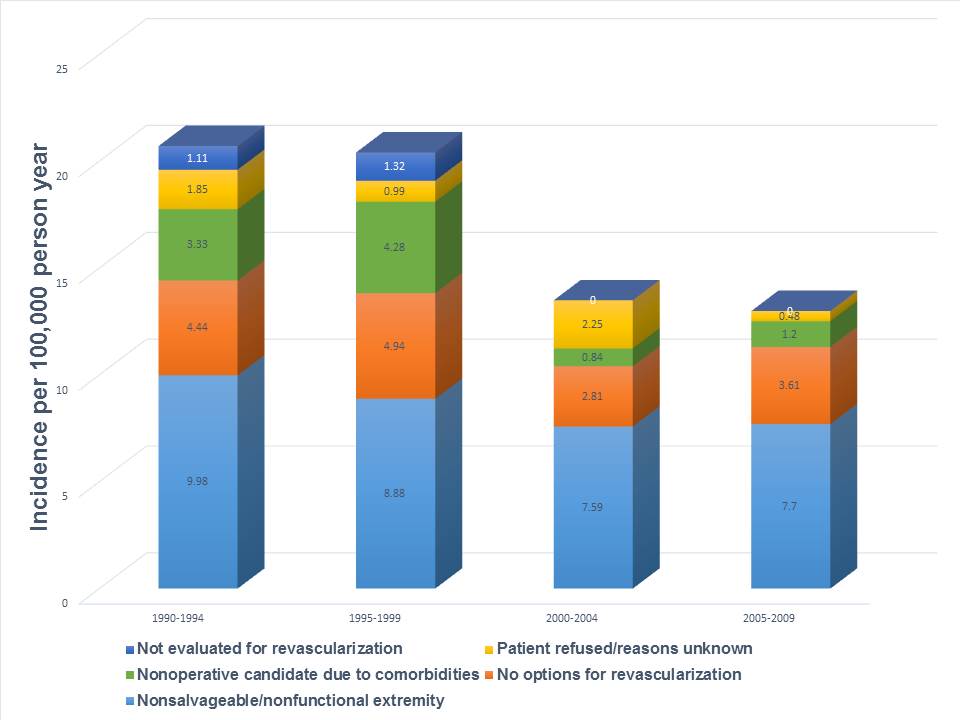
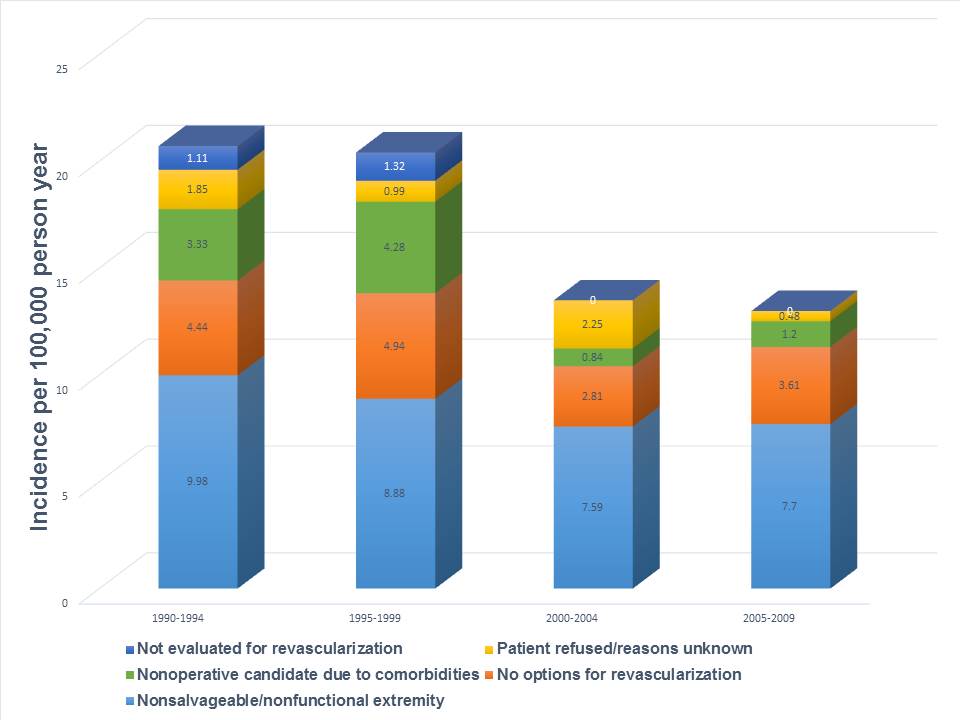
There were 773 patients (1168 limbs) with PAD; 622 patients (955 limbs) underwent revascularization procedures. There were 220 person limbs (190 patients), 58.5% males with mean age 72 years (range 31-97) that underwent PA. The overall incidence of amputation (per 100,000 person-years) declined from 20.7 in 1990-94 to 13 in 2005-09 ( p=0.0123). All patient demographics remained stable over the study period with the exception of an increase in the prevalence of obesity (BMI≥40, 1.8 % to 12.5 %, p=0.02) and non-white race (1.2% to 12.5%, p=0.02) in the population. There was no decline in the most frequent indications for PA ; non-salvageable/non-functional limb (51.3%) and no option for revascularization (23.6%). Of PA limbs 3.2 % had no vascular evaluation before amputation; the incidence of this decreased significantly over time (1.1 to 0 per 100,000 person.years, p<0.0001). Revascularization was refused in 13.7% considered non-operative candidates due to co-morbidities; with a decreasing trend in this factor (3.3 to 1.2 per 100,000 person.years, p =0.26). Failure to revascularizae due to patient refusal and unknown reasons accounted for 8.2% of PAs. Figure 1.
Conclusion:
In a long term population based study of patients with peripheral arterial disease the incidence of primary amputation decreased significantly over time, with significant decline in lack of vascular evaluation. Non salvagebale limbs and no-option patients still account for the majorty of PA’s and shoud be targeted for further efforts to decrease amputations.
Back to 2016 Annual Symposium Abstacts
|