|
Back to 2016 Annual Symposium Abstacts
Long-term Outcomes of Thoracic Endovascular Aortic Repair
Jocelyn M. Beach, MD, Yuki Kuramochi, RN, BSN, Corey Brier, MA, Eric E. Roselli, MD, Matthew J. Eagleton, MD.
Cleveland Clinic, Cleveland, OH, USA.
OBJECTIVES:
Long-term data regarding the safety and durability of thoracic endovascular aortic repair (TEVAR) is limited. The objective of this study was to evaluate the long-term outcomes of thoracic endografts in high-risk patients with descending thoracic aortic pathology.
METHODS:
High-risk patients were treated with thoracic endografts (2001-2011) under a prospective, physician-sponsored investigational device exemption trial. Three-dimensional reconstructions and measurements were performed on computed tomography scans acquired prior to discharge, at 1-, 6-, and 12-months then yearly thereafter. Kaplan-Meier analysis was used to assess survival and freedom from re-intervention.
RESULTS:
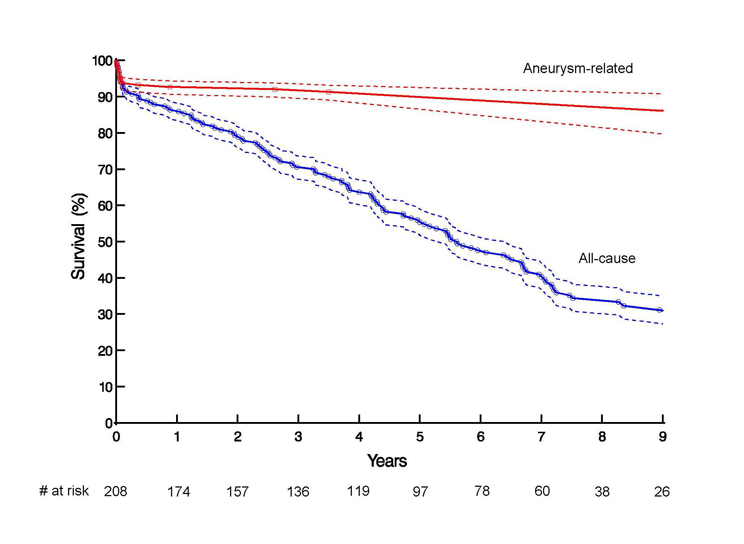
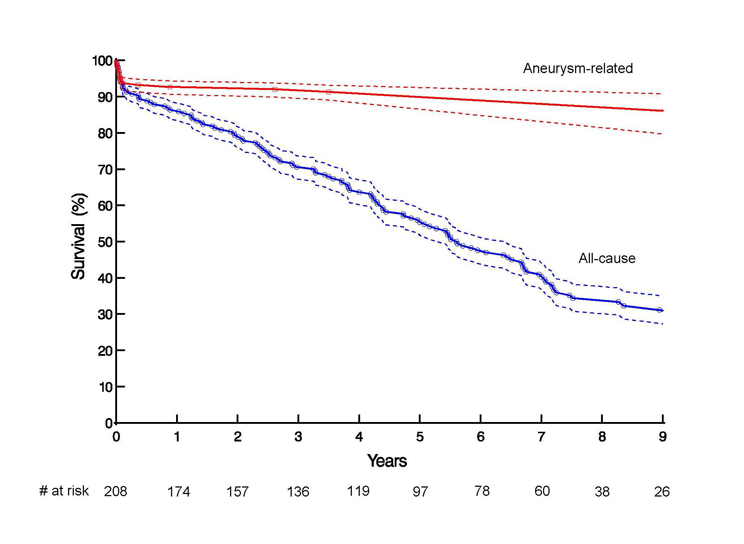
Of the 208 patients, 171 were treated for thoracic aneurysm, 28 for chronic dissection, 8 for symptomatic aortic ruptures, and 1 for aortic fistula. Fifty-six patients (26.9%) had prior aortic repair and 84 (40.3%) required surgical modification for adequate landing zone. Patients were followed for an average of 4.8±3.3 years with 97 (46.6%) followed for >5 years. Operative mortality was 6.2%, and survival at 30-days, 1-, 5-, and 9-years was 94.2%, 86.4%, 55.4%, and 31.1%, and freedom from aneurysm-related death was 94.2%, 91.3%, 91.3%, 92.0%, respectively (Figure). Sixty-six endoleaks occurred in 57 patients (28.2% of 202 with eligible imaging), with 31 primary (≤ 30 days) and 35 secondary (> 30 days) endoleaks. Aneurysm growth (>5mm) was noted in 16 patients, with first point of growth noted at a median 3.3 years (IQR 2.0-5.2 years). There were 5 patients who developed component separation, 3 of which were treated with stent-grafts, and 14 patients with barb or stent fractures for which 1 associated re-intervention was performed. Seventy-five re-interventions were performed in 55 patients, with overall freedom from re-intervention at 30-days, 1-, 5-, and 8-years of 88.8%, 81.9%, 74.1%, and 62.7%, respectively. Fifty-three (71%) of re-interventions were thoracic aneurysm-related, 40 (75%) of which were endovascular procedures. Thirty-five of these were to correct endoleaks with median time of 1.5 years (IQR 0.1-6.1 years).
CONCLUSIONS:
When implanted according to strict anatomic criteria, TEVAR devices are durable and associated with high long-term aneurysm-related survival. Long-term imaging follow-up remains critical to identify endoleaks or rare device durability issues, most of which can be monitored or managed with endovascular therapies.
Back to 2016 Annual Symposium Abstacts
|