|
Back to 2016 Annual Symposium Abstacts
Impact of Thoracic Endovascular Repair on Aortic Pulsatile Changes in Patients with Thoracic Aortic Aneurysm Pathologies
Foeke JH Nauta, MD1, Guido HW van Bogerijen, MD, PhD1, Chiara Trentin, PhD2, Michele Conti, PhD3, Frans L. Moll, MD, PhD4, Joost A. van Herwaarden, MD, PhD4, Ferdinando Auricchio, PhD2, Santi Trimarchi, MD, PhD1.
1Policlinico San Donato IRCCS, University of Milan, Milan, Italy, 2CESNA Center for Advanced Numerical Simulations, Istituto Universitario di Studi Superiori di Pavia (IUSS), Pavia, Italy, 3Department of Civil Engineering and Architecture, Structural Mechanics Division, University of Pavia, Pavia, Italy, 4Department of Vascular Surgery, University Medical Center Utrecht, Utrecht, Netherlands.
OBJECTIVES:
The impact of thoracic endovascular aortic repair (TEVAR) on aortic pulsatile changes remains unclear. Our objective was to study both distensibility (radial changes) and extensibility (longitudinal changes) during the cardiac cycle before and after TEVAR, potentially clarifying stent graft related complications.
METHODS:
Custom developed software and 4-dimensional computed tomography angiography, obtained during the cardiac cycle, were used to measure area, diameter and length changes in eight patients treated with TEVAR for thoracic aortic aneurysm pathologies. Distensibility and extensibility were calculated by the area and length differences divided by the baseline area and length, respectively.
RESULTS:
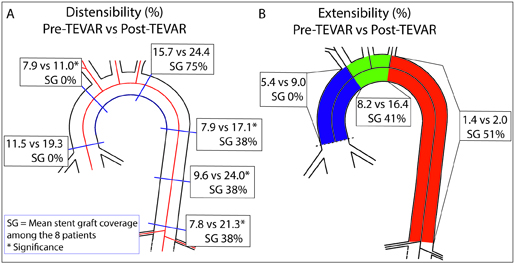
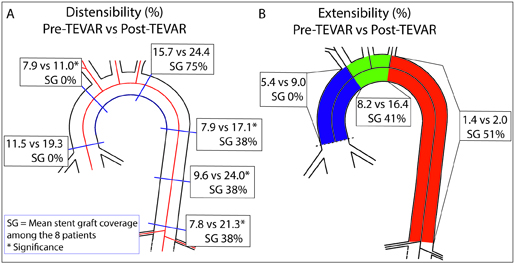
The majority of patients were males (75%; mean age 71.0 ± 8.2 years). Significant distensibility and extensibility was observed at all levels during the cardiac cycle, both pre- and postoperatively. After TEVAR, aortic distensibility increased at the level of the brachiocephalic trunk (P = .03), at the levels 10 cm (P = .04) and 20 cm distal (P = .01) to the left subclavian artery, and at the level of the celiac trunk (P = .01, Figure 1A). Aortic extensibility was preserved after TEVAR and showed a trend of increase in the ascending aorta (P = .06) and the aortic arch (P = .07, Figure 1B). In addition, the total thoracic aortic length, from the aortic root till the celiac trunk, increased after TEVAR from 387.9 ± 38.2 mm to 395.4 ± 33.8 mm, P = .046).
CONCLUSIONS:
We observed an increase of distensibility and a trend of increased extensibility, marked proximal to the stent graft, after TEVAR. This observation might imply that forces on thoracic aortic stent grafts are greater than currently realized, which may have implications for stent graft design and related complications.
Back to 2016 Annual Symposium Abstacts
|