|
Back to 2016 Annual Symposium Abstacts
Percutaneous Intervention for Carotid In-stent Re-stenosis (C-ISR) Does Not Improve Outcomes Compared to Non-operative Management
Jayer Chung, MD, Wilmer Valentine, MD, Sherene Sharath, MPH, Neal R. Barshes, MD, MPH, George Pisimisis, MD, Panagiotis Kougias, MD, Joseph L. Mills, MD.
Michael E. DeBakey Veterans Affairs Medical Center, Baylor College of Medicine, Houston, TX, USA.
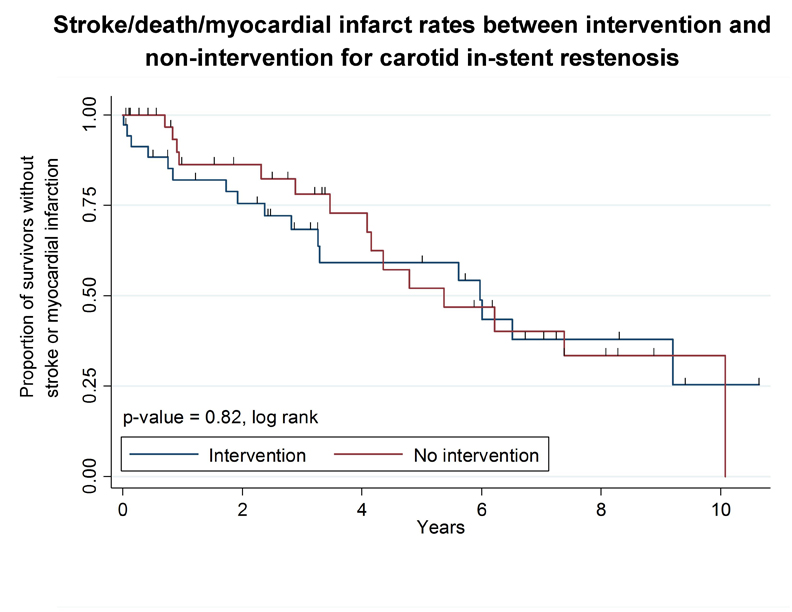
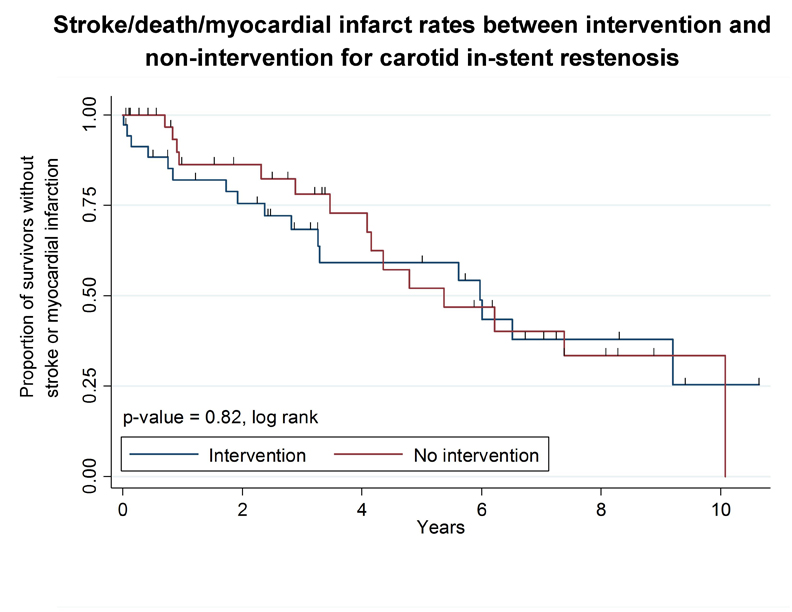
Objective: Indications for intervention for moderate-to-severe (> 50% by NASCET criteria) carotid in-stent re-stenosis (C-ISR) are unclear. We therefore sought to compare stroke/death/myocardial infarction (MI) rates between percutaneous interventions and non-operative management for > 50% C-ISR.
Methods: We performed a single-center retrospective review of consecutive patients presenting with > 50% C-ISR to the Vascular Surgery Service. Demographic, comorbidities, intra-operative and postoperative variables were obtained. The degree of stenosis was verified by review of digital subtraction, or computed tomographic angiograms. The primary outcome was stroke/death/MI after the diagnosis of > 50% C-ISR. χ2, Kruskal-Wallis, and Kaplan-Meier analysis was utilized to quantify outcomes between the patients treated percutaneously versus non-operatively.
Results: Over a ten year period, 75 patients presented with > 50% C-ISRs (N=74 male, 98.7%; N=57 asymptomatic, 76.0%) with a median age of 67.5 years (62.8, 74.6). The initial pathology underlying the original stent was atherosclerosis in 33 (70.2%); radiation-induced in 10 (21.3%) and prior carotid endarterectomy (CEA) in 4 (8.51%) and unknown in 28 (37.3%). Forty-seven patients underwent a percutaneous intervention (30 percutaneous angioplasty (PTA) only, 63.8 %; 17 repeat stent and PTA, 36.2%). Median-follow up for the entire cohort was 59.6 months (19.5, 133.3), and similar between the intervention and non-intervention arms. There were no significant differences between the arms with respect to age (p=0.16), medical co-morbidities (p > 0.05), original stent type (p-0.46), or clopidogrel utilization (p=0.74). At thirty-days, stroke/death/MI, was higher in the intervention arm yet the length of stay was higher in the non-intervention arm (p=0.03). During the follow up period, a median of 1.0 procedure was required to maintain patency. By Kaplan-Meier analysis, there were no statistically significant differences between the intervention and non-intervention arms with respect to stroke/death/MI at last follow-up (p=0.82). One-year Kaplan-Meier-estimated patency was superior in the intervention versus the non-intervention arm (117.9 days + 76.8 versus 77.7 days + 99.1; p=0.02).
Conclusions: For > 50% C-ISR, percutaneous interventions fail to improve long-term stroke/death/MI rates relative to non-intervention, though long-term patency is improved. Future appropriately powered, prospective non-inferiority trials may confirm these findings.
Back to 2016 Annual Symposium Abstacts
|