|
Back to 2016 Annual Symposium Abstacts
Preoperative Inflammatory Status as a Predictor of Primary Patency Following Femoropopliteal Stent Implantation
Kenneth R. Nakazawa, BS, Sean P. Wengerter, MD, Robert A. Lookstein, MD, Rami O. Tadros, MD, Windsor Ting, MD, Michael L. Marin, MD, Peter L. Faries, MD, Ageliki G. Vouyouka, MD.
Division of Vascular Surgery, Icahn School of Medicine at Mount Sinai, New York, NY.
OBJECTIVE:
To evaluate the impact of preoperative inflammatory status, as determined by complete blood count (CBC) test parameters, on 12 and 24-month patency of femoropopliteal stenting for peripheral arterial disease.
METHODS:
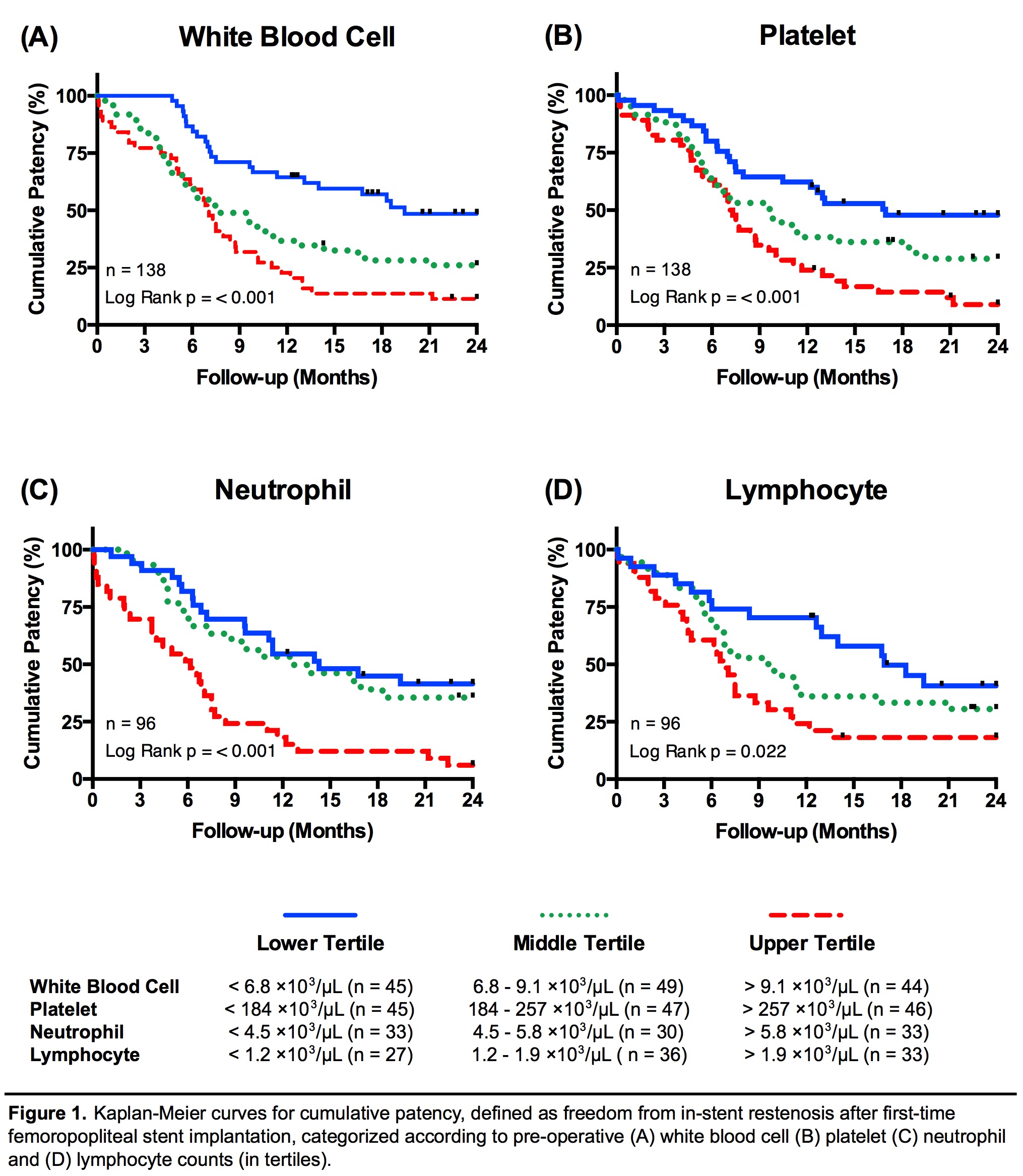
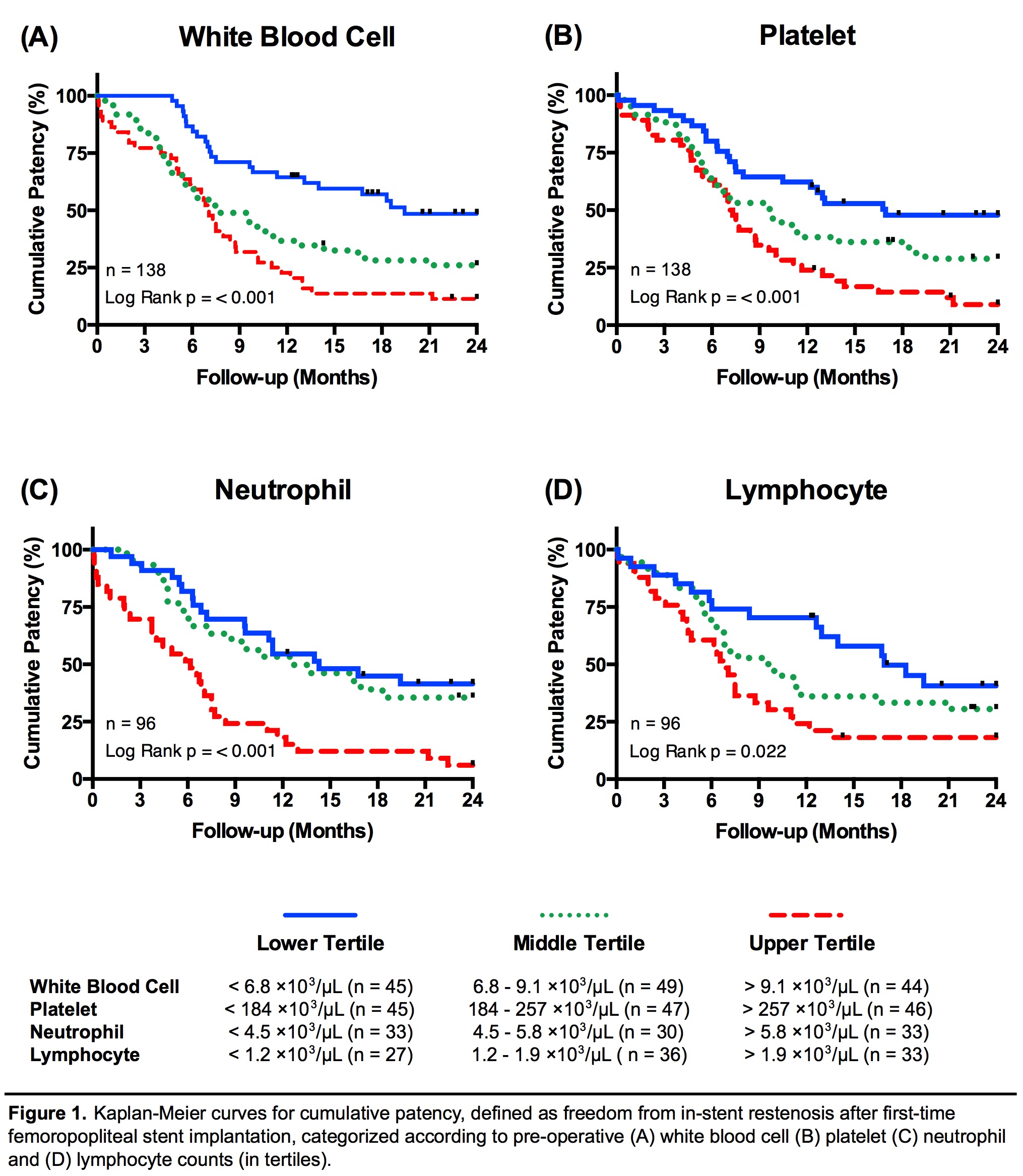
We retrospectively analyzed baseline clinical and angiographic data among 138 patients (median age: 73 years, 46% females) from 2005-2015 at our institution with preoperative CBC test values and information of patency for at least 12 months after first-time femoropopliteal stenting. Patients were stratified into tertiles based on pre-procedural counts to evaluate associations with ISR (Figure 1). The primary endpoint was loss of primary patency, defined by a Doppler velocity ratio ≥2.5:1, computed tomographic angiography demonstrating ≥50% luminal narrowing within the stent, or re-intervention.
RESULTS:
During a median follow-up of 22 months, 81 patients (59%) had in-stent restenosis (ISR) within 12 months and significantly higher preoperative white blood cell (WBC), platelet, neutrophil, and lymphocyte counts than 57 patients (41%) whose stents remained patent for longer than 12 months (p<0.01). Compared with patients in the lower WBC tertile (n=45, median patency: 19.4 months), those in the upper WBC tertile (n=44) had a median patency of 7.0 months and a 3.3-fold increased adjusted risk for ISR (p<0.001). Compared with patients in the lower platelet tertile, (n=45, median patency: 16.9 months), those in the upper platelet tertile (n=47) had a median patency of 7.1 months and a 2.7-fold increased adjusted risk (p=0.001). Compared with patients in the lower neutrophil tertile (n=33, median patency: 14.3 months), those in the upper neutrophil tertile (n=33) had a median patency of 6.2 months and a 3.2-fold increased adjusted risk (p=0.001). After adjusting for covariates, patients divided into tertiles by lymphocyte counts exhibited no significant differences for ISR. The final Cox proportional hazards model included age, sex, lesion type, TASC II score, vessel runoff, anti-platelet therapy, presence of diabetes, critical limb ischemia, adjunct procedures, hyperlipidemia, and end-stage renal disease.
CONCLUSIONS:
Routine pre-procedural tests that determine baseline inflammatory status may provide strong clinical utility in assessing potential patient risk stratification for ISR after femoropopliteal stenting. Circulating WBCs, platelets, and neutrophils may be important inflammatory mediators of ISR.
Back to 2016 Annual Symposium Abstacts
|