|
Back to 2016 Annual Symposium Abstacts
Preoperative Beta Blockers Reduce Postoperative Bleeding in Open AAA Repair
Tammam Obeid, MD, Isibor Arhuidese, MD, Caitlin Hicks, MD, Besma Nejim, MD, Mahmoud Malas, MD.
Johns Hopkins Medical Institutions, Baltimore, MD, USA.
OBJECTIVES: Current practice guidelines of open abdominal aortic aneurysm (AAA) repair are optimized towards reducing cardiac events and lowering mortality. However, non-cardiac complications, specifically postoperative bleeding, remain under studied outcomes that have significant impact on in-hospital mortality, patient morbidity and medical costs.
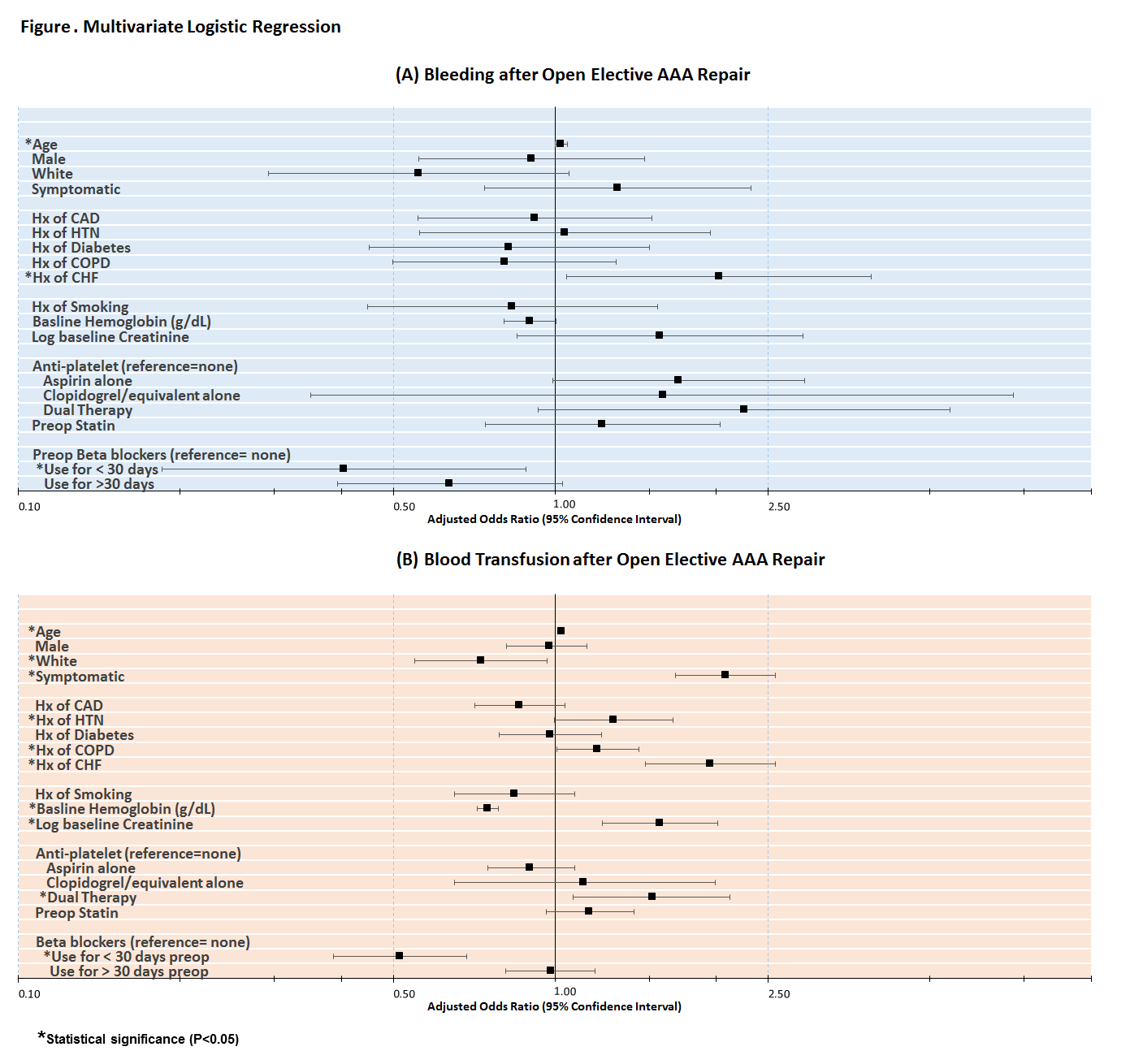
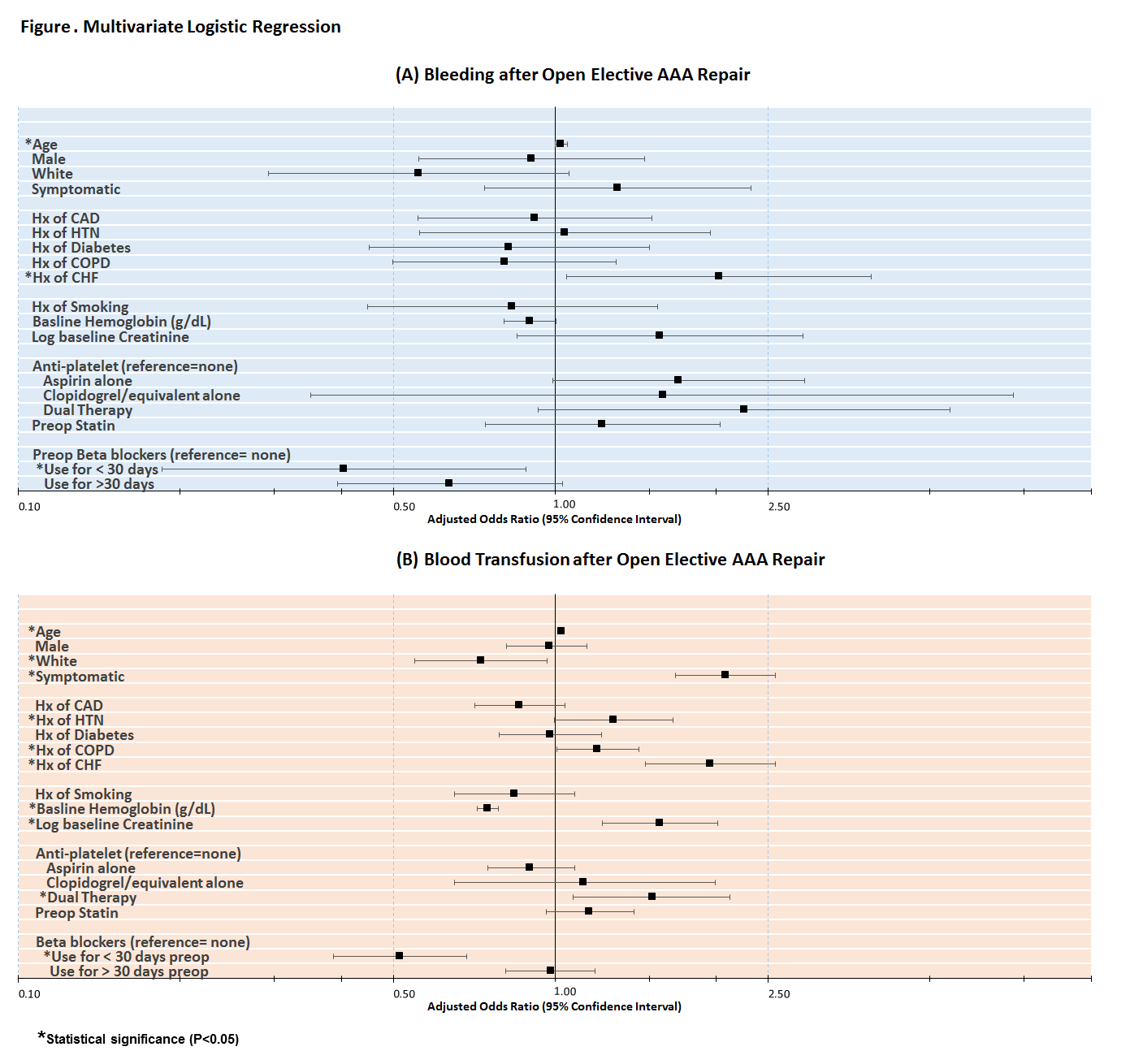
METHODS: We analyzed all patients who underwent elective open AAA repair between 2003-2014 in the Vascular Quality Initiative database. Multivariate logistic regression models were constructed to assess the effects of age, gender, race, comorbidities, smoking, symptomatic status, renal function, preoperative hemoglobin, and pre-operative medication (aspirin, statins, and beta blockers) on postoperative bleeding requiring return to operating room and postoperative blood transfusion of >3 units.
RESULTS:
A total of 4,789 patients underwent elective open AAA repair during the 12-year period (mean age 69.6±0.13 years, 73% males). In-hospital mortality rate was 3.2%, while perioperative (30-day) mortality rate was 3.5%. Total in-hospital complications rate was 44.1%; cardiac (myocardial infarction; congestive heart failure; dysrhythmia) complications rate was 17.2% and non-cardiac (bleeding; transfusion; bowel or leg ischemia; respiratory-related; wound-related; renal impairment) complications rate was 36.7%. Postoperative bleeding requiring return to OR occurred in 2.2% of cases, while blood transfusion of >3 units was needed in 18.6% of patients.
Beta blocker use for 1-30 days preoperatively was associated with 60% reduction in postoperative bleeding (OR 0.40, 95%CI 0.19-0.88, P=.02) and 50% decrease in blood transfusion risk (OR 0.51, 95%CI 0.39-0.68, P<.001).
Dual anti-platelet therapy increased the likelihood of postoperative transfusion by more than 50% (OR 1.52, 95%CI 1.08-2.12, P=.02).
An increase in baseline hemoglobin by 1 g/dL was associated with a 25% decrease in transfusion need after open AAA (OR 0.75, 95%CI 0.72-0.79, P<.001), while being white had about 30% reduction in postoperative blood transfusion (OR 0.73, 95%CI 0.55-0.97, P=.03).
Other significant predictors of outcomes included age, symptomatic status, baseline creatinine level, congestive heart failure, hypertension and COPD (all, P<0.05; Figure).
CONCLUSIONS: Preoperative beta blocker use is associated with reduced risk of postoperative bleeding and blood transfusion in open elective AAA repair. This could be due to better hemodynamic control. Beta blockers use in reducing non-cardiac morbidity, specifically within average risk patients, deserves further investigation.
Back to 2016 Annual Symposium Abstacts
|