Back to 2016 Annual Symposium Abstacts
The Incidence and Effect of Conical Necks During EVAR in the GREAT Registry
William P. Shutze, Sr., John Kedora, Steve Hohmann, Brad Grimsley, Dennis Gable, Greg Pearl, John Eidt, Bert Smith.
The Heart Hospital Baylor Plano, Dallas, TX, Texas Vascular Associates, Dallas, TX.
OBJECTIVES:Conical necks of abdominal aortic aneurysms (AAA) are an increase in the diameter of the proximal landing zone (LZ) by at least 2 mm. This anatomy may require the use of aortic cuffs, be associated with a higher re-intervention rate and vary in regards to the associated neck angle and overall neck diameter. We used the data in the Gore Global Registry for Endovascular Aortic Treatment (GREAT) to evaluate the incidence and effects of conical necks in endovascular aneurysm repair (EVAR) for AAA.
METHODS: This analysis was performed on subjects with AAA treated from August 2010 until an August 10th, 2015 data export. Conical neck was defined as those with a maximum minus the minimum proximal aortic LZ diameter >2mm. Demographics, comorbidities, anatomic details, aortic cuff extender use, hospital length of stay, postoperative intervention (all and device related (DR)) and endoleak data were extracted. Percent conical neck score (%CNS) was calculated as the diameter difference/ minimum aortic diameter.
RESULTS:
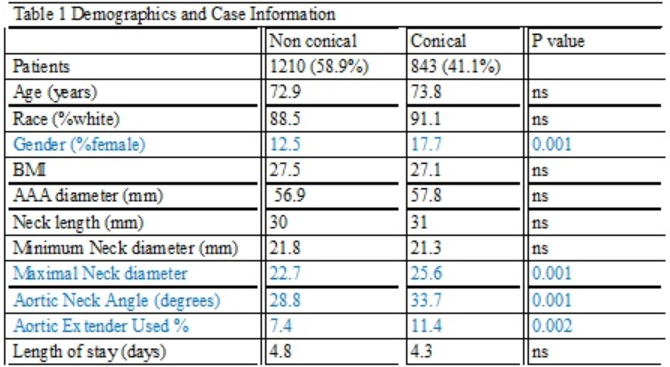
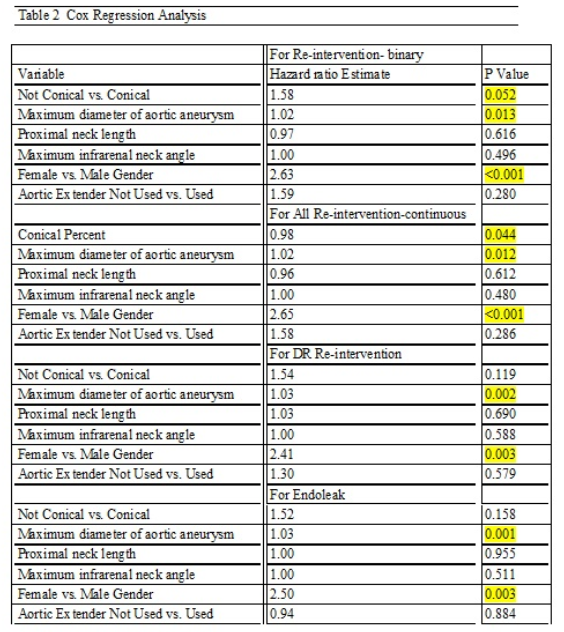
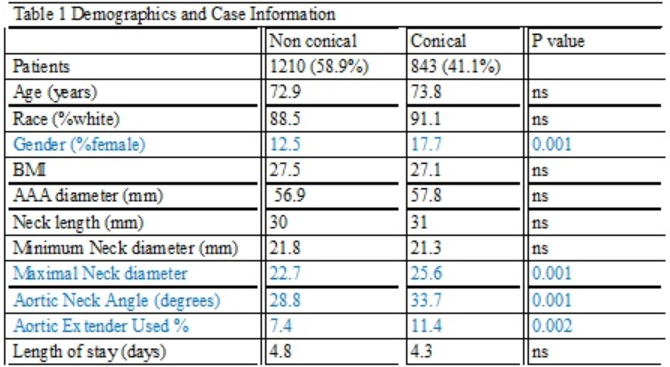
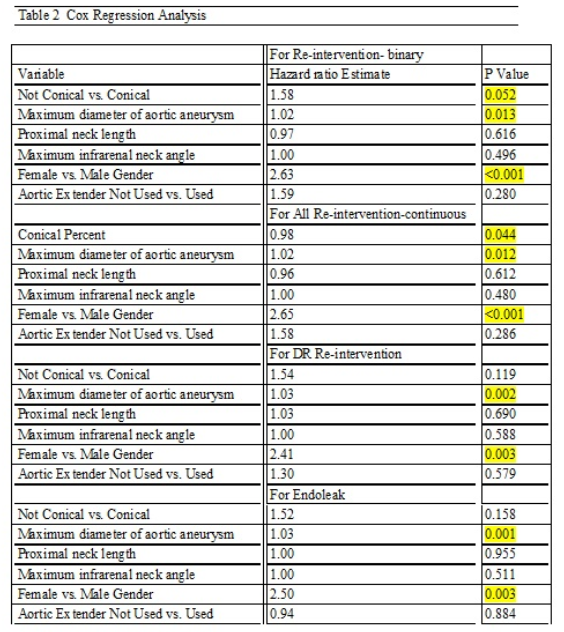
There were 2053 subjects: 1053 (58.9%) with N-CN and 843 (41.1%) with CN (Table 1). The two groups were comparable for age, race and BMI, postoperative length of stay, AAA diameter, neck length, minimum proximal aortic diameter but differed in gender, maximum proximal aortic diameter, infrarenal aortic neck angle and aortic extender use. The mean % CNS was 20.7% with a range of 6.8-129.4%. Post-procedure follow-up time for the two groups was 417 + 410 (N-CN) and 337 + 364 days (CN). Cox multivariate regression models for binary and continuous CN in regards to re-intervention, and endoleak demonstrated that CN, neck length and neck angle were not risk factors for re-intervention but AAA diameter and female gender were.
CONCLUSIONS:CN is more common in females and is associated with increased use of aortic extenders but does not increase the LOS or increase the risk of re-intervention and device related re-intervention. AAA diameter and female gender are associated with increased need for re-intervention and endoleak.
Back to 2016 Annual Symposium Abstacts
|