|
Back to 2016 Annual Symposium Abstacts
Anatomic Severity of Abdominal Aortic Aneurysm is Related to Patient and Hospital Value for Patients Undergoing Endovascular Repair
Lauren E. Trakimas, D.O., Doran S. Mix, M.D., Khurram Rasheed, M.D., Claudia I. Aghaie, B.S., Jennifer L. Ellis, M.D., Roan J. Glocker, M.D., Adam A. Doyle, M.D., Michael C. Stoner, M.D..
University of Rochester, Rochester, NY, USA.
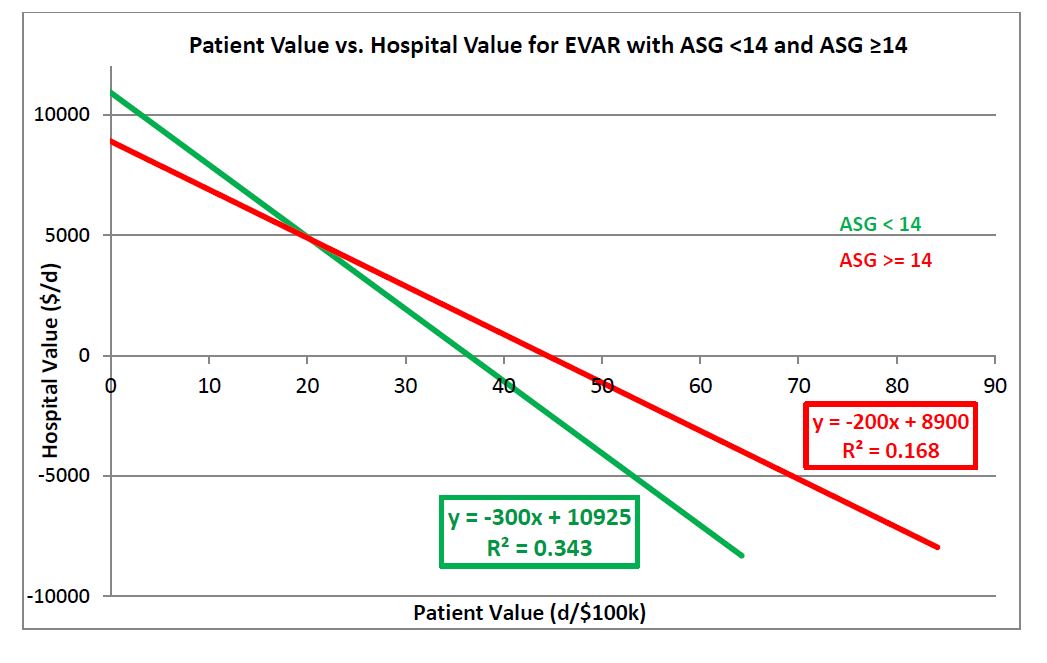
OBJECTIVES:It has previously been shown that higher anatomic severity grade (ASG) is correlated with operative complexity and resource utilization. However, current reimbursement in aortic surgery is based on procedure volume and does not account for anatomic complexity or patient outcome. Our study compared the relationship between hospital value (HV) and patient value (PV) for endovascular aortic repair (EVAR). We hypothesized that anatomic severity impacts the patient-hospital value relationship.
METHODS: Patients who underwent elective EVAR were identified. Pre-operative CT angiograms were reviewed and ASG score was assigned. Patient with ASG < 14 were defined as being in the simple group while those with ASG ≥ 14 were defined as the complex group. Patient comorbidity profile was quantified using a modified Charleston Comorbidity Index (mCCI). Cost and contribution margin were used to define patient and hospital value respectively, as we have previously described. Linear regression was used to compare patient value [(freedom from complication (days) + mCCI) / net revenue (\0 ] to hospital value [contribution margin (\0 / length of stay (days)].
RESULTS: 173 patients with complete clinical and financial data were included in our analysis. Mean age was 72.88 ± 0.68, with no significant difference between race, mCCI, or medication profile (beta-blockers, statins, ASA, Plavix, and ACE inhibitors). Male gender and number of adjunct procedures (endograft repositioning, limb extension, branch vessel embolization) were significantly different between groups (p < 0.01). Linear regression modeling demonstrated that PV was negatively correlated to HV. Patients in the simple group had a higher correlation of PV and HV than those in the complex group (slope= -300, R2= 0.343 and slope = -200, R2= 0.169). EVARs with lower ASG scores had the better value correlation (Figure).
CONCLUSIONS:These data clearly demonstrate that patient and hospital value are not correlated in contemporary reimbursement systems. However, hospital value and patient value are better aligned when anatomic morphology is more favorable. Furthermore, higher ASG is significantly correlated with likelihood of adjunct procedures. Dramatic changes in hospital and surgeon reimbursement will be required to sustain EVAR in a value-based healthcare system.
Back to 2016 Annual Symposium Abstacts
|






