|
Back to 2016 Annual Symposium Abstacts
Cost-Effectiveness of Catheter-Directed Thrombolysis Compared to Systemic Thrombolysis for the Treatment of Massive Pulmonary Embolism
Elizabeth A. Genovese, MD MS, Nathan L. Liang, MD, Kenneth J. Smith, MD, MS, Efthymios Avgerinos, MD, PhD, Michel S. Makaroun, MD, Rabih A. Chaer, MD, MSc.
University of Pittsburgh Medical Center, Pittsburgh, PA, USA.
OBJECTIVES:Acute massive pulmonary embolism (PE) is associated with high morbidity and mortality. Systemic thrombolysis (ST) may improve survival compared to anticoagulation alone, but is associated with high rates of hemorrhagic complications. Catheter directed thrombolysis (CDT) has emerged as an alternative therapy that is associated with reduced hemorrhagic complications but is associated with a higher procedure cost. The objective of this study was to evaluate the cost effectiveness of CDT compared to ST.
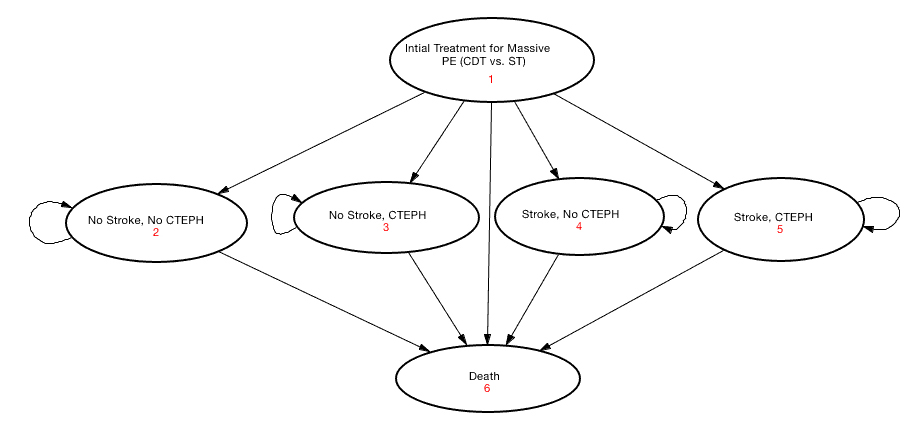
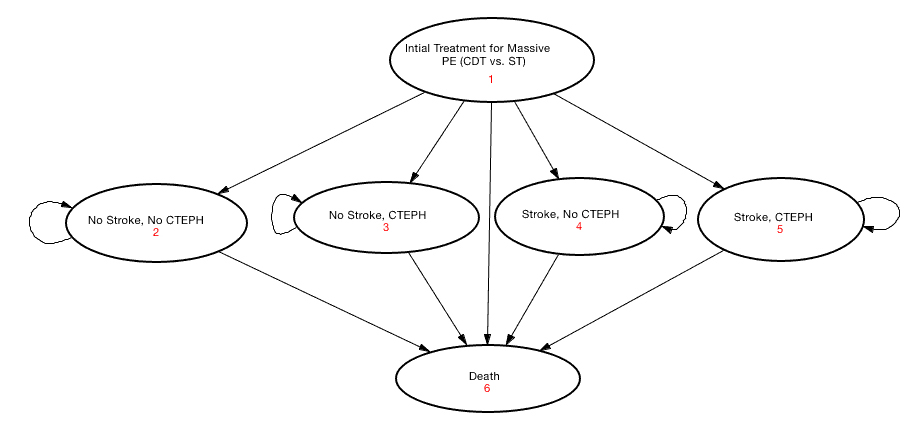
METHODS: A Markov state-transition model comparing CDT to ST was created to simulate patient-oriented outcomes including clinical improvement, major hemorrhagic complications, long-term outcomes (e.g., chronic thromboembolic pulmonary hypertension[CTEPH] and disability from a major stroke), and quality adjusted life years (QALY); see Figure 1 for state-transition diagram.
 The base case was a 60 year old male presenting with an unprovoked massive PE. We took a societal perspective with a 5-year time horizon. Parameter estimates were derived from published literature and extracted from the National Inpatient Sample (2009-2012). Costs were adjusted to 2013 US dollars. The base case was a 60 year old male presenting with an unprovoked massive PE. We took a societal perspective with a 5-year time horizon. Parameter estimates were derived from published literature and extracted from the National Inpatient Sample (2009-2012). Costs were adjusted to 2013 US dollars.
RESULTS: Initial treatment costs were estimated at \,774 for CDT and \,610 for ST. At 5 years, CDT was associated with an incremental cost effectiveness ratio of \,108 per QALY gained compared to ST. One-way sensitivity analyses demonstrated that CDT was favorable at a threshold of \,000/QALY gained when its initial treatment cost remained under \,073 or if CDT mortality, major hemorrhage or stroke rates remained less than 8.9%, 12.9% and 1%, respectively. CDT also remained favorable when initial ST costs exceeded \,309 or if rates of mortality, major hemorrhage or stroke rates for ST exceeded 12.3%, 7.2% or 1.5%, respectively. Probabilistic sensitivity analysis favored CDT in 56.3% of model iterations at a willingness to pay threshold of \,000/QALY.
CONCLUSIONS:While CDT has a higher initial procedural cost compared to ST, it is also associated with decreased mortality and major hemorrhagic complication rates, particularly intracranial hemorrhage, and subsequently is a more cost effective treatment strategy for massive PE.
Back to 2016 Annual Symposium Abstacts
|