Back to 2016 Annual Symposium Abstacts
Percutaneous EVAR in Morbidly Obese Patients
Jason A. Chin, MD, Laura Skrip, MPH, Bauer Sumpio, MD, PhD, Jonathan Cardella, MD, Jeffrey Indes, MD, Timur Sarac, MD, Alan Dardik, MD, PhD, Cassius I. Chaar, MS, MD.
Yale New Haven Hospital, New Haven, CT, USA.
OBJECTIVES:
The advantages of percutaneous endovascular aortic aneurysm repair (PEVAR) compared to femoral cutdown (CEVAR) are demonstrated in previous publications. Morbidly obese (MO) patients present unique anatomical challenges and have not been specifically studied. This study examines the trends in the use of PEVAR and its surgical outcomes compared to CEVAR in MO patients.
METHODS:
The ACS-NSQIP files for the years 2005-2013 were reviewed. All MO patients (BMI ≥ 40) undergoing EVAR were included in the comparison groups. Patients were included in the CEVAR group if they had any one of 23 selected CPT codes describing an open femoral procedure. The PEVAR group included any remaining patients who had only CPT codes for EVAR and endovascular procedures. The trends in use of PEVAR were described as percentage of total EVARs performed in MO patients per year. The 2 groups were compared for baseline comorbidities and surgical outcomes using chi-square or t-test as appropriate.
RESULTS:
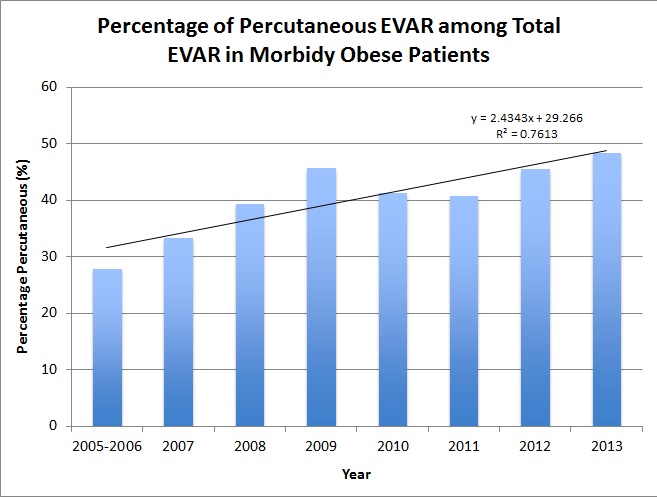
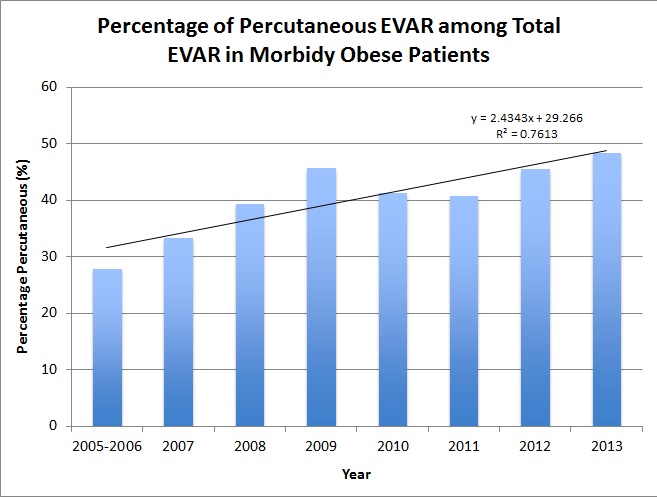
There were 887 MO patients (CEVAR=507, PEVAR=380) constituting 3.2% of all patients undergoing EVAR. The use of PEVAR in MO patients significantly increased from 28% of total EVARs in 2005/6 to 48% in 2013 (P=0.037; Figure 1). There were no differences in baseline characteristics between the 2 groups including age, comorbidities, and emergent procedures. There was no difference in the mean BMI (CEVAR=45.3 vs PEVAR=44.9). PEVAR patients had shorter duration of anesthesia (242 vs 269 minutes; P=0.002), shorter total operation time (161 vs 179 minutes; P=0.001), and shorter length of hospital stay (3.5 vs 4.6 days; P=0.007). PEVAR had a trend towards decreased wound complications (6.1% vs 9.6%; P=0.051). There was no difference in any other complication or mortality. A subgroup analysis of 117 super obese patients with BMI ≥50 (CEVAR=65, PEVAR=52) demonstrated a shorter hospital stay for PEVAR (3.2 days vs 5.6 days; P=0.008) and no difference in operating time or wound complications.
CONCLUSIONS:
PEVAR is increasingly used in MO patients and decreases operating time and hospital stay. The advantages of a percutaneous approach to EVAR seem to decrease in the super obese patients.
Back to 2016 Annual Symposium Abstacts
|