|
Back to 2016 Annual Symposium Abstacts
Outcomes for Symptomatic Abdominal Aortic Aneurysms (sAAA) in the American College of Surgeons National Surgical Quality Program (ACS-NSQIP)
Peter A. Soden, MD, Sara L. Zettervall, MD, Klaas HJ Ultee, BS, MPH, Jeremy D. Darling, BA, Katie E. Shean, MD, Sarah E. Deery, MD, Allen D. Hamdan, MD, Marc L. Schermerhorn, MD.
Beth Israel Deaconess Hospital, Boston, MA, USA.
OBJECTIVES:
Historically sAAAs had intermediate mortality compared to asymptomatic (aAAA) and ruptured AAAs (rAAA) but recent results, with wider EVAR use, suggest mortality of sAAA repair is similar to aAAA. Prior studies were limited by small numbers. In this study we evaluate mortality with sAAA repair in a large contemporary population.
METHODS:
All patients undergoing infrarenal AAA repair in the 2011-2013 ACS-NSQIP, Targeted Vascular module, excluding embolization, dissection, thrombosis, or acute conversions to open repair were identified. 30-day mortality and major adverse events (MAE) were compared for EVAR and open repair, stratified by presentation, by univariate and multivariable analysis.
RESULTS:
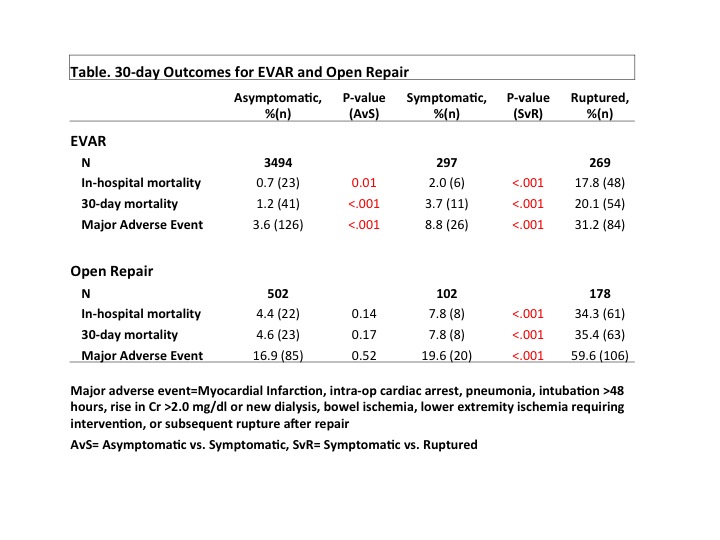
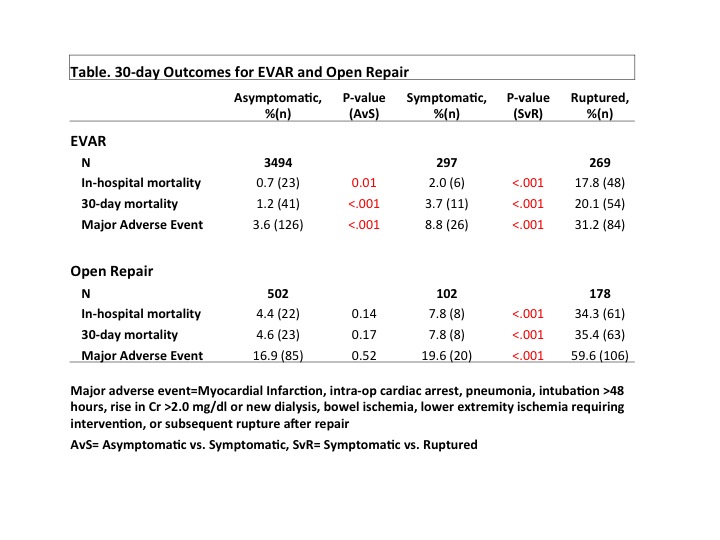
4842 infrarenal AAAs were identified, 3996 asymptomatic (502 open repair, 3494 [87%] EVAR), 399 symptomatic (102 open, 297 [74%] EVAR), and 447 ruptured aneurysms (178 open, 269 [60%] EVAR). Aneurysm diameter was similar between aAAA and sAAA (5.8cm ±1.2 vs. 5.9cm ±1.7, p=.13) but larger for rAAA (7.7cm ±2.1 , p<.001). Proportion of females was similar in sAAA and rAAA (26% vs. 21%, p=.12, respectively), but lower in aAAA (14%, p=.001). sAAA and aAAA had lower 30-day mortality after EVAR and open repair compared to rupture (Table). With EVAR, sAAA had higher 30-day mortality (3.7% vs. 1.2%, p<.001; adjusted OR 2.7, 95%CI 1.3-5.5) and MAE rates (8.8% vs. 3.6%, p<.001) compared to aAAA. Following open repair, sAAA 30-day mortality trended higher (7.8% vs. 4.6%, p=.17; adjusted OR 1.8, 0.8-4.2) compared to aAAA. Combining EVAR and open repairs in adjusted analysis; sAAAs were twice as likely to die within 30-days (OR 2.4 95%CI 1.3-3.9) and 1.5 times as likely to have a MAE (OR 1.5 95%CI 1.02-2.2) when compared to aAAA.
CONCLUSIONS:
sAAA patients had higher rates of 30-day mortality and MAE compared to aAAA. This difference was most pronounced after EVAR, showing that peri-op mortality for sAAA is still intermediate between aAAA and rAAA. Also, half the deaths following EVAR of aAAAs and sAAAs occur after discharge.
Back to 2016 Annual Symposium Abstacts
|