|
Back to 2016 Annual Symposium Abstacts
Long-Term Improvement in Outcomes Following Carotid Endarterectomy is Associated with Statin Use
Sapan S. Desai, MD, PhD, MBA, Sarah Koch, MD, James Pan, MD, Douglas Hood, MD, Kim J. Hodgson, MD.
Southern Illinois University, Springfield, IL, USA.
OBJECTIVES:
NASCET, ACAS, and CREST have better characterized the role of carotid endarterectomy (CEA) for treating severe carotid artery disease. However, the impact of statins on long-term outcomes after surgery has not previously been quantified. The purpose of this study is to evaluate the association between statin use and long-term outcomes following CEA.
METHODS:
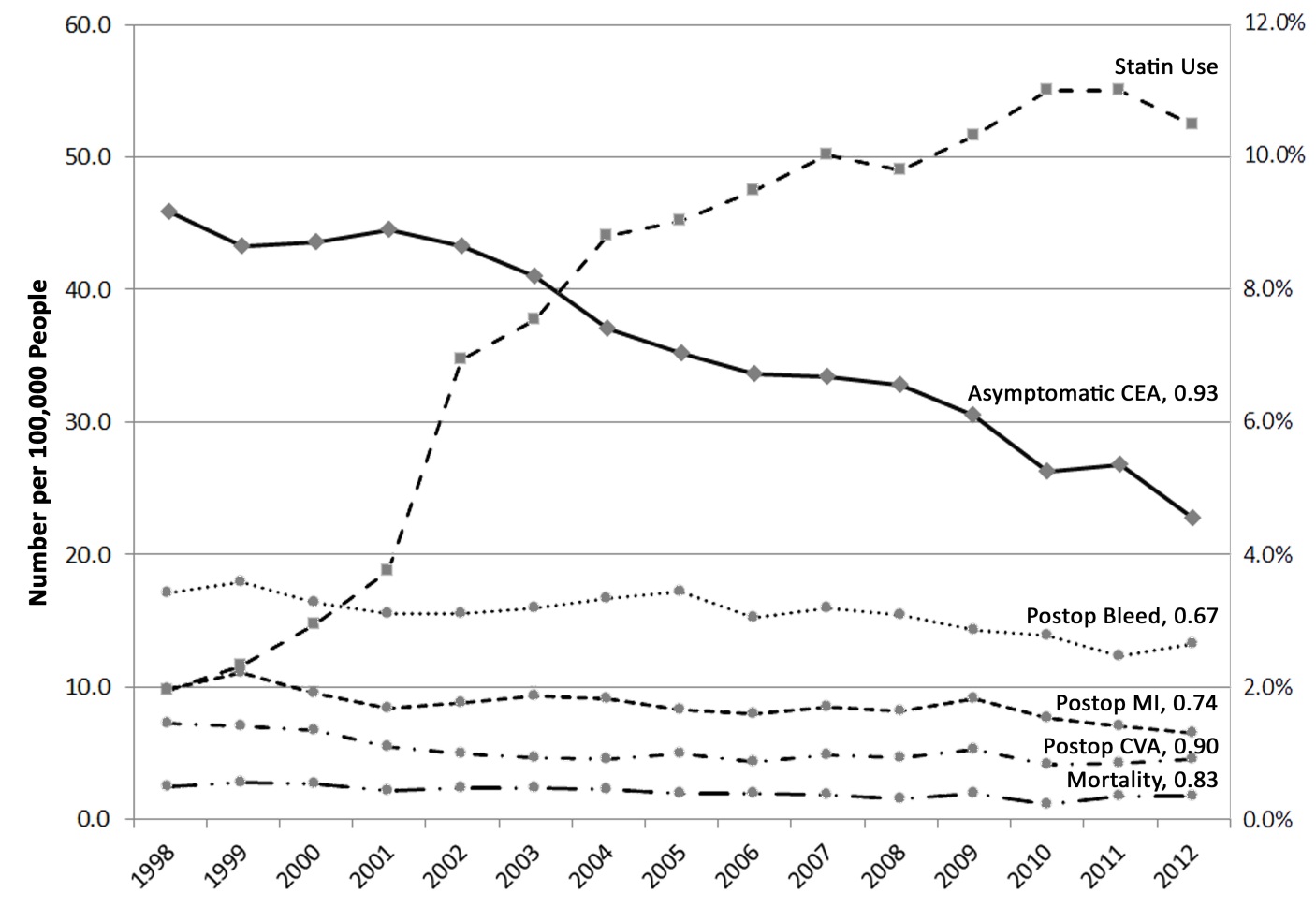
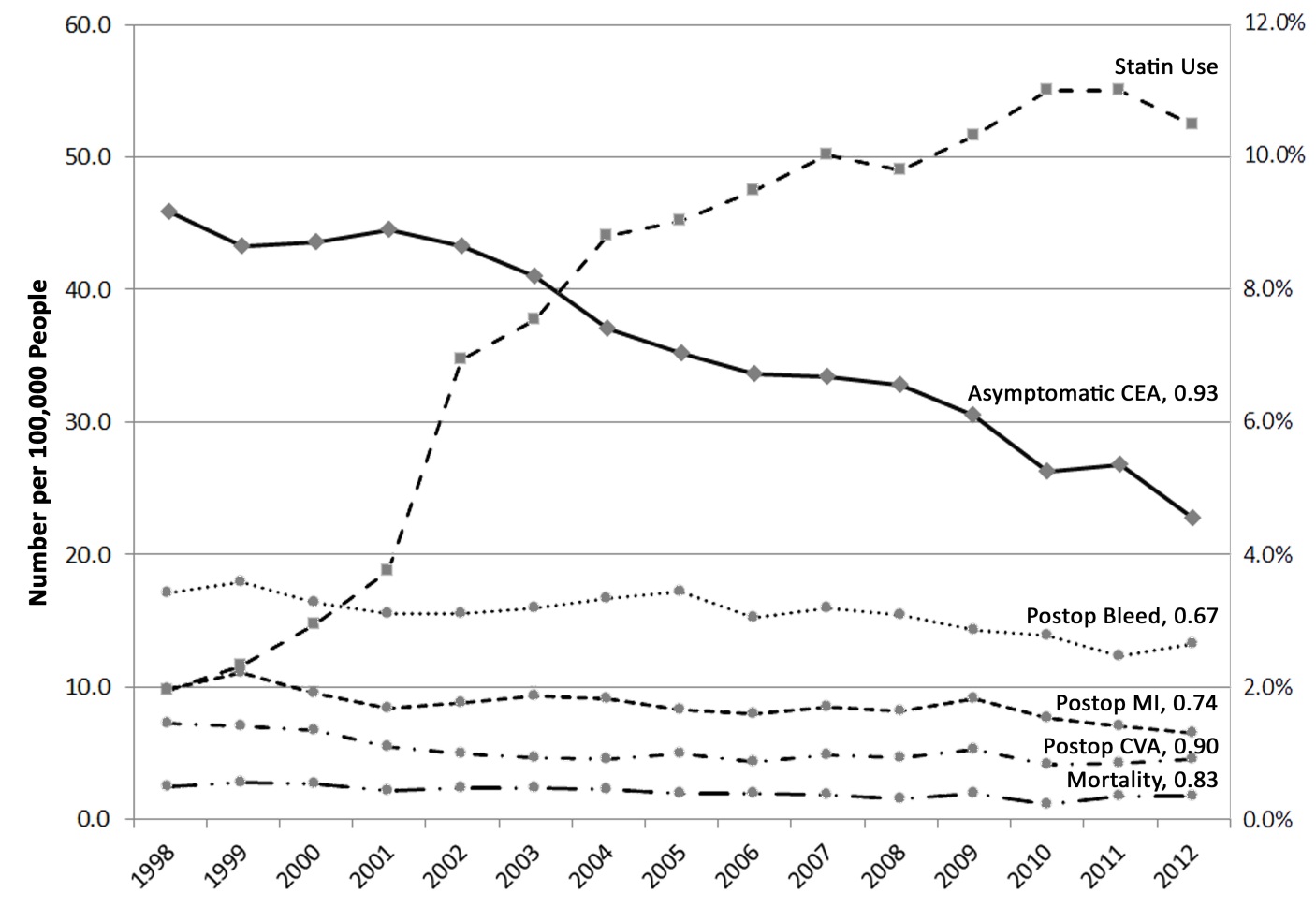
Patients who underwent CEA at our institution from 2013-2015 were identified and characterized by demographics, comorbidities, and symptoms. Outcome measures included postoperative bleeding, myocardial infarction (MI), stroke (CVA), mortality, length of stay (LOS), and cost of care. Comparison to national data was done using the AHRQ National Inpatient Sample (NIS) and State Inpatient Databases (SID) from 1998-2012. Statin use was characterized through the Medical Expenditure Panel Survey and institutional data. Pearson correlations are presented as coefficients of determination (r2) with significance at P<0.05. Trend analysis was completed using the Mann-Kendall test.
RESULTS:
A total of 1,583,616 patients who underwent CEA were identified through the AHRQ databases. From 1998-2012, statin use increased from 2.0% to 10.5%. In this period, postoperative bleeding (3.4% to 2.6%), MI (2.0% to 1.3%), CVA (1.4% to 0.9%), and inpatient mortality (0.5% to 0.3%) decreased (P<0.01 on trend analysis). This decrease was strongly correlated to statin use for postoperative bleeding (r2 = 0.67, P<0.01), postoperative MI (r2 = 0.74, P<0.01), postoperative CVA (r2 = 0.90, P<0.001), and inpatient mortality (r2 = 0.83, P<0.001). At our institution, 81/118 (68.1%) were on a statin preoperatively and 3/118 (2.5%) developed a postoperative complication (1 bleeding, 1 MI, 0 CVA, and 1 death). Statin use was associated with shorter LOS (1.1 +/- 0.4 days vs. 2.2 +/- 2.4 days, P<0.01), lower cost of care (\,756 savings per patient, P<0.01), and fewer complications (0/81 vs. 3/37). Routine statin use was associated with a decrease in volume of CEA (44% decline from 1998 to 2012, r2 = 0.93, P<0.001).
CONCLUSIONS:
Routine statin use is strongly associated with improved outcomes, shorter LOS, and lower costs at both the institutional and national levels. Increased statin utilization may further decrease the incidence of significant carotid artery disease.
Back to 2016 Annual Symposium Abstacts
|