|
Back to 2016 Annual Symposium ePosters
Relationship between Endovascular Revascularization Trends, Surgical Training, Infrapopliteal Bypass Volume and Outcomes in Patients with Limb-Threatening Ischemia (LTI)
Jayer Chung, MD, Sherene Sharath, MPH, Neal R. Barshes, MD, MPH, George Pisimisis, MD, Panagiotis Kougias, MD, Joseph L. Mills, MD.
Michael E DeBakey Veterans Affairs Medical Center, Baylor College of Medicine, Houston, TX, USA.
Objective: Increasingly, endovascular therapies are utilized to treat limb-threatening ischemia (LTI). The impact of this trend upon trainee education and outcomes for infrapopliteal bypasses (IPBs) remains unclear.
Methods: Single-institution, retrospective review of all consecutive revascularizations performed for LTI. Demographic, comorbidities, intra-operative and postoperative outcomes, and trainee-level were abstracted. Trends in trainee volume, co-morbidities, demographics, operative, perioperative, and one-year outcomes were analyzed. Single and multiple linear regressions quantified associations between IPB and the aforementioned variables.
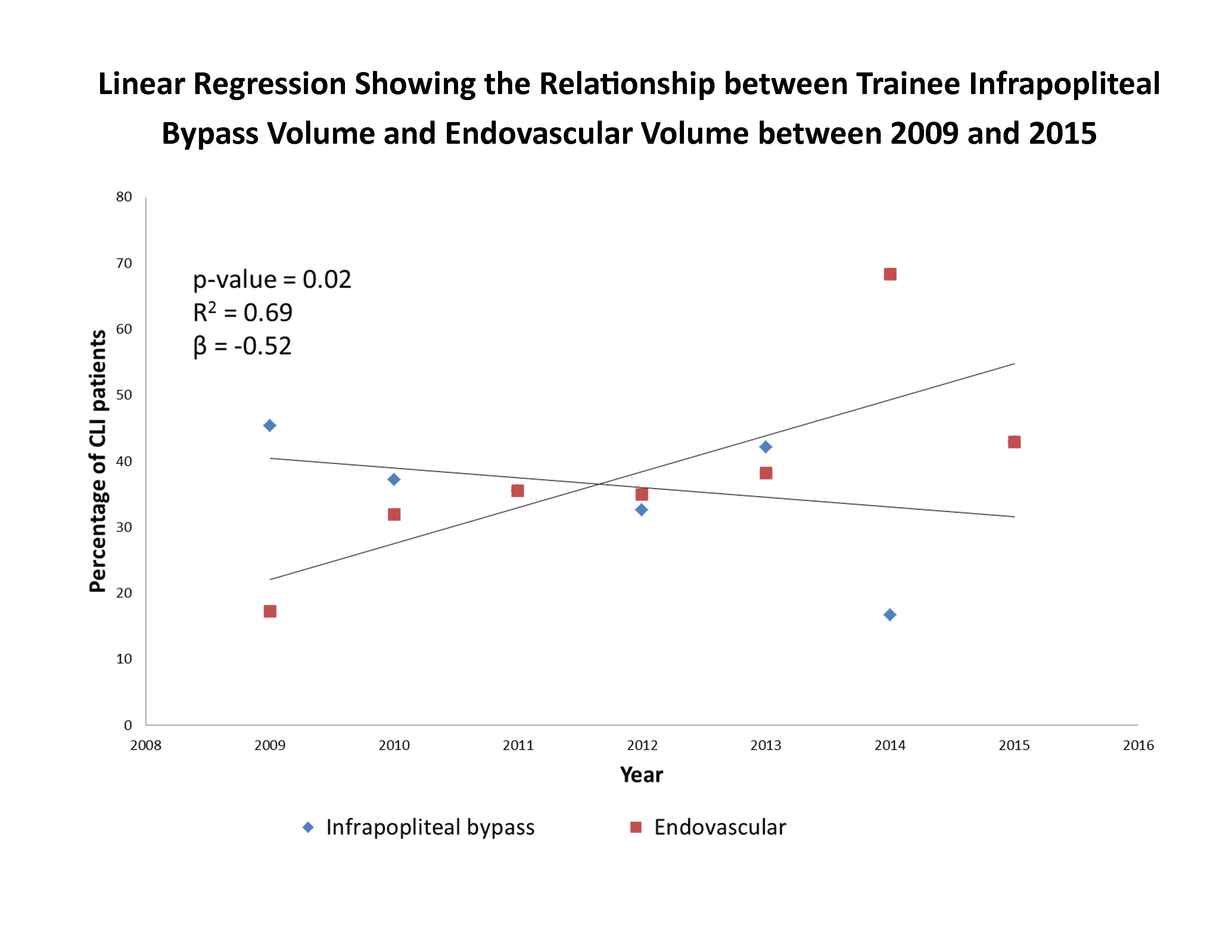
Results: Over 62 months, 537 procedures were performed (N=339 open, 63%) upon 428 subjects (N=427 male, 99.7% male) for mostly tissue-loss (N=345, 65%). 272 (51%) procedures were infrapopliteal (N=192, 71% open; N=80, 29% endo). Among endovascular interventions, the number of infrapopliteal procedures increased (p < 0.01) with a contemporaneous decrease in the number of infrainguinal bypasses overall (IIB; p=0.05) and IPBs (p=0.05). While the number of IPBs performed by vascular fellows decreased (p = 0.63), the largest decreases occurred among general surgery chief and junior residents, whose experience decreased from N=18 in 2009 to N=1 in 2015 (p < 0.01.) The prevalence of coronary artery disease (p=0.03) and current tobacco abuse (p=0.02) in IPB subjects decreased significantly, with an increase in the median age (p=0.05). All other variables failed to show an association with time in the IPB group. Median operative time increased significantly for IPBs (p 0.35 each). One-year major amputation rates and mortality decreased significantly, while amputation-free survival increased (p < 0.01 each) for both IPB and endovascular infrapopliteal procedures. One-year graft patency was unchanged over time. Multiple linear regression showed only the number of endovascular procedures/month was associated with the decline in the number of IP bypasses/month (β= -0.52, 95% CI= -0.92, -1.20; R2=0.69; p=0.05).
Conclusions: Increasing endovascular revascularizations are most strongly associated with decreasing IPB volumes for all trainees, especially general surgery residents. While the trends are associated with improved outcomes, a persistent need for IPB remains. Training programs may need to adjust IPB training to maintain outcome standards and prevent a loss of comparability with endovascular revascularizations. 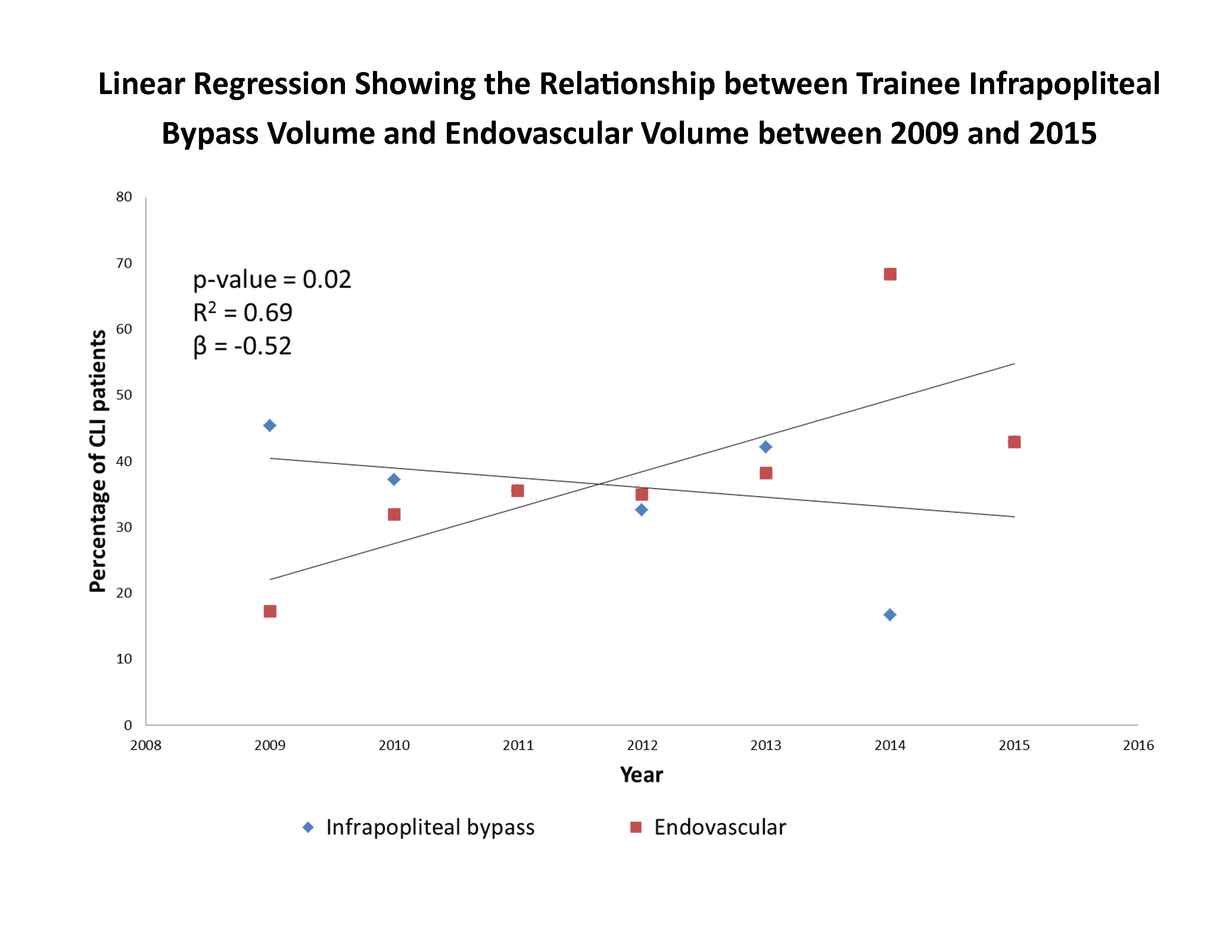
Back to 2016 Annual Symposium ePosters
|