|
Back to 2016 Annual Symposium ePosters
Abdominal Visceral Fat Correlates with Adverse Outcomes in Open but not Endovascular Aortic Repair
Lauren E. Trakimas, D.O., Doran S. Mix, M.D., Claudia I. Aghaie, B.S., Khurram Rasheed, M.D., Jennifer L. Ellis, M.D., Roan J. Glocker, M.D., Adam A. Doyle, M.D., Michael C. Stoner, M.D..
University of Rochester, Rochester, NY, USA.
OBJECTIVES: Abdominal visceral fat, rather than subcutaneous fat, has been associated with higher risk of heart disease, hypertension, diabetes mellitus type 2, and the metabolic syndrome. Visceral fat is thought to represent an overall increase in inflammatory state. Furthermore, formation and enlargement of abdominal aortic aneurysms (AAA) is associated with pro-inflammatory mediators. We hypothesized that visceral fat area (VFA), not subcutaneous fat area (SFA) is an independent predictor of post-operative complications after AAA repair.
METHODS: Patients who underwent elective infrarenal endovascular aortic repair (EVAR) and open repair were identified. Demographic characteristics of age, gender, race, comorbidities, and medication profile were obtained. Pre-operative CT angiograms were reviewed. SFA and VFA (cm2) were measured in the axial view at the third lumbar vertebrae using a Hounsfield Unit (HU) restricted region growth algorithm. Post-operative complications were defined, including 30-day mortality, and a composite complication score (CCS) was assigned for the presence of any complication or death. A univariate analysis was performed on the above variables. Then a multivariate analysis was conducted for both open and EVAR to analyze the independent effect of the pre-operative and comorbid characteristics affecting CCS.
RESULTS: A total of 271 patients were identified. Mean age was 72.66 ± 0.54, 82% were male, and 94% were Caucasian. Mean VFA was 247± 7.81 cm2. Ninety patients were identified as having a CCS event. Significant patient factors in initial univariate analysis included hyperlipidemia, statin use, and age (Table). In multivariate analysis, VFA was significantly associated with CCS in open repair (p = 0.02), but not EVAR (p=0.16). SFA was not associated with CCS for either open (p = 0.45) or EVAR (p = 0.83).
CONCLUSIONS: This study shows that VFA is an independent predictor of poor outcomes in open AAA repair, not EVAR. The effect of VFA was significantly seen on multivariate analysis. The same effect was not seen for SFA. A patient’s overall comorbid state, as represented by VFA, should be taken into consideration when selecting patient and approach for elective repair. 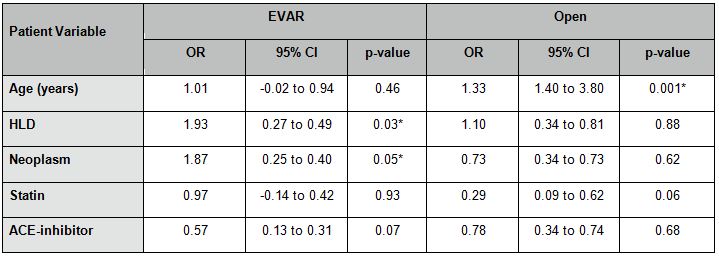
Back to 2016 Annual Symposium ePosters
|






