|
Back to 2016 Annual Symposium ePosters
Endosalvage Techniques - Relining of Infrarenal EVAR as a Solution for High-Pressure Endoleak
Tazo Inui, MD1, Erik Owens, MD2, Dennis Bandyk, MD1, John S. Lane, MD1, David Rigberg, MD3, Andrew Barleben, MD1.
1UC San Diego, San Diego, CA, USA, 2VAMC San Diego, San Diego, CA, USA, 3UC Los Angeles, Los Angeles, CA, USA.
OBJECTIVE - Management of endoleaks after endovascular aneurysm repair (EVAR) remains a vexing problem. Aneurysm remodeling may lead dynamic stress upon the graft seal zones leading to delayed endoleak. If the graft cannot accommodate this, the weakest portion of the graft will be exploited, potentially leading to a high-pressure endoleak. Candidates for re-intervention for endoleak clearly include: Type 1 or Type 3 endoleaks, or indeterminate endoleaks with symptoms/aneurysm growth, all of which can lead to aneurysm re-pressurization/rupture. Techniques for repair include open conversion for endograft failure, conversion to an aorto uni-iliac repair or adding endovascular cuffs/extensions in piecemeal fashion. We believe graft relining with a complete second endograft from renal artery origin to iliac bifurcation is the most appropriate management.
METHODS - Four patients required relining of Endologix Powerlink or AFX with a Gore Excluder or Trivascular Ovation endograft. We had 100% technical success with placement and resolution of high-pressure endoleak/symptoms/aneurysm growth.
RESULTS - Of the 4 patients, there was 1 Type 1A, 3 Type 3 endoleaks, and 1 Type 5 with rapid aneurysm growth. One patient had a Type 1A and concomitant Type 3A endoleak. Two patients had undergone previous attempts at repair. Changes following initial EVAR included an average increase in renal artery-aortic bifurcation centerline measurement of 12 mm, mean aortic neck diameter growth of 2.7 mm, and a mean aneurysmal diameter increase of 8 mm. Mean follow-up was 385 days following relining. No morbidity/mortality was noted. One Type 2 endoleak was observed. All aneurysms halted growth or showed a diameter decrease.
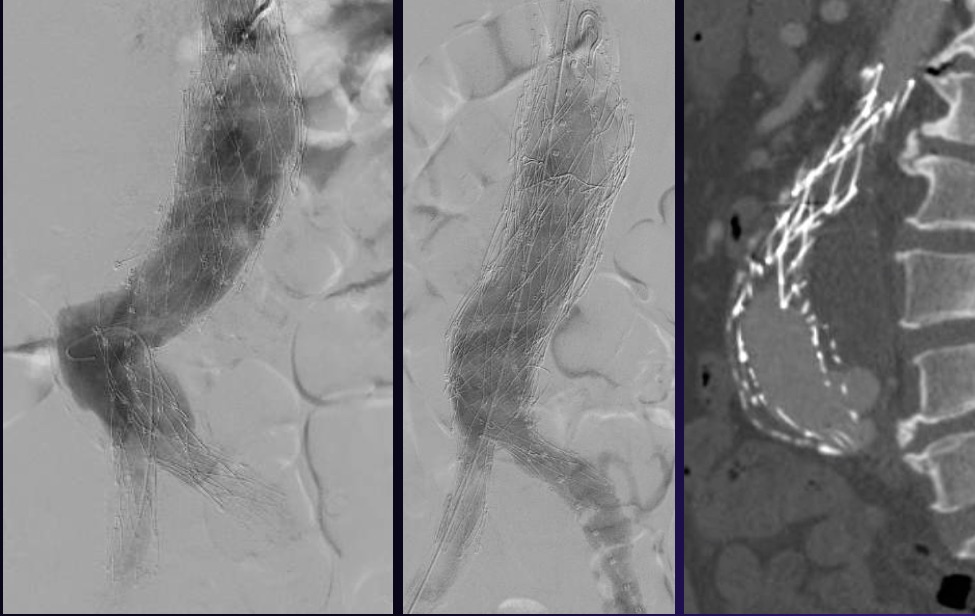
CONCLUSIONS - Controversy remains regarding the appropriate management of endoleak following EVAR. Aortic remodeling may contribute and is poorly understood. There are an increasing number of endosalvage techniques available. Technical and durable success is associated with freedom from a reportedly high morbidity and mortality (20%). We describe our institution’s “real-world” endovascular method for re-excluding the aneurysm. 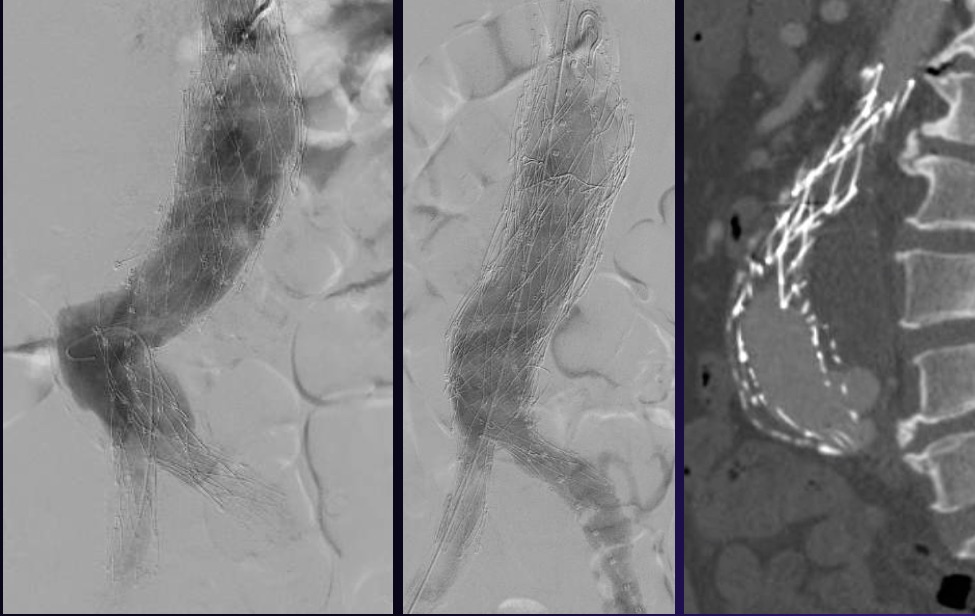 Figure 1. A. 2 years following EVAR with 3 normal CT’s prior, B repair with cuff and palmas stent, C Following a normal CT, patient continued to have aortic remodeling and developed a new type 3 endoleak. Figure 1. A. 2 years following EVAR with 3 normal CT’s prior, B repair with cuff and palmas stent, C Following a normal CT, patient continued to have aortic remodeling and developed a new type 3 endoleak.
Back to 2016 Annual Symposium ePosters
|