|
Back to 2016 Annual Symposium ePosters
Sequential Catheterization and Stenting Amid Progressive Deployment of the Zenith® t-Branch™ device for Branched Endovascular Aortic Aneurysm Repair
Carlos H. Timaran, MD1, David Timaran1, Juan Gomez, MD2, Gabriel Mejia, MD3, Juan Carbonell, MD4, Pierre Galvagni, MD5.
1University of Texas Southwestern Medical Center, Dallas, TX, USA, 2Clinica CardioVID, Medellin, Colombia, 3Clinica Universitaria Colombia, Bogota, Colombia, 4Fundacion Valle del Lili, Cali, Colombia, 5Universidad Federal de Santa Catarina, Florianapolis, Brazil.
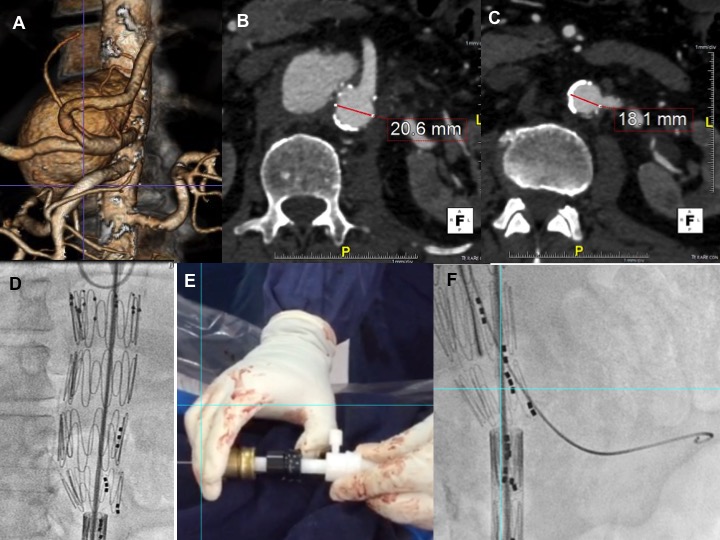
Objectives: Branched endovascular aneurysm repair (BEVAR) is an alternative to open repair of thoracoabdominal aortic aneurysms (TAAAs). Unfavorable anatomy, including a narrow aortic lumen (Fig.A-C), is often a limiting factor for BEVAR. The Zenith® t-Branch™ is an off-the-shelf device designed for treating TAAAs. The purpose of this study was to assess technical success of BEVAR using a sequential catheterization/stenting amid progressive t-Branch deployment in patients with unfavorable anatomy.
Methods: Over a 12-month period, 22 patients (12 men) underwent BEVAR using the Zenith® t-Branch™ device. Sequential deployment was used in 8 patients (5 men). Each branch was released sequentially while the distal part of the device was maintained constrained within the sheath (Fig.D). The proximal end of the device was opened by slightly displacing the control knobs (Fig E). Each target vessel was catheterized and stented sequentially (Fig. F). Technical success was defined as complete exclusion of the aneurysm sac with successful catheterization and patent branched visceral arteries.
Results: Median age was 72 years(interquartile range[IQR], 64-81). Narrow aortic lumen 60°). A narrow true lumen (<25 mm in diameter) was present in 2 patients (25%) with dissecting TAAAs. Median aneurysm size was 6.2cm(IQR, 5.5-8.4). Aneurysms were classified as type II (50%), type III (25%) or type IV (25%). Technical success for stenting all target vessels arteries was 100%. In 2 patients, 2 branches were purposely unstented for sac perfusion. These branches were successfully stented 3 weeks later. In one case, the t-Branch was unintentionally deployed in the false lumen. Access to the visceral vessels required fenestration of the septum through the branches using a transeptal needle. Median procedure time was 265 minutes(IQR, 168-348); median fluoroscopy time 73 minutes(IQR, 51-86); median contrast load 103cc(IQR, 91-130); and estimated blood loss 250cc(IQR, 125-550). No 30-day mortality occurred. No periprocedural paraplegia or strokes occurred.
Conclusions: BEVAR using sequential deployment and stenting of the t-Branch device is safe and effective in the treatment of complex TAAAs in patients with narrow aortic lumen or unfavorable anatomy. 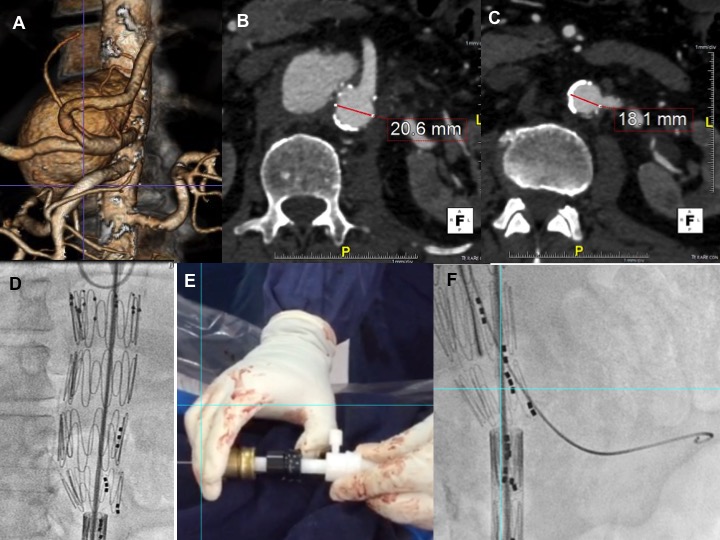
Back to 2016 Annual Symposium ePosters
|