|
Back to 2016 Annual Symposium ePosters
Endovascular versus Open Repair of Ruptured Abdominal Aortic Aneurysm
Alykhan M. Lalani, MS1, Shvetank Agarwal, MD, FASE2, Brice Hwang, BS1, George Mckelvey, PhD3, Gautam Agarwal, MD2.
1Medical College of Georgia at Georgia Regents University, Augusta, GA, USA, 2Georgia Regents University Health Center, Augusta, GA, USA, 3Detroit Medical Center, Detroit, MI, USA.
OBJECTIVES: Ruptured aortic aneurysms (rAAA) may be managed either endovascularly (EVAR) or with open repair (OR). Management of hemodynamically unstable rAAAs is still not clear. The purpose of this study was to describe the management of rAAAs at our institution over the past 7 years and to compare the outcomes of EVAR versus OR.
METHODS: Upon institutional review board approval, patients undergoing rAAA treatment in our institution between July 2007 and December 2014 were identified and their electronic medical records reviewed. Data collected included demographics, clinical presentation, treatment modality, complications and late outcomes. Early mortality was the primary outcome measure recorded, with secondary outcome measurements being operative blood loss, blood products administered during surgery, and postoperative complications. Data was analyzed using ANOVA tests (unpaired T-test) for continuous variables (presented as means ± S.D) and Chi-squared tests (presented as % and raw case numbers) for categorical data. All factors were entered into a forward stepwise logistic regression model to identify predictors of adverse RAA procedure outcomes. A p value of > 0.05 was considered statistically significant.
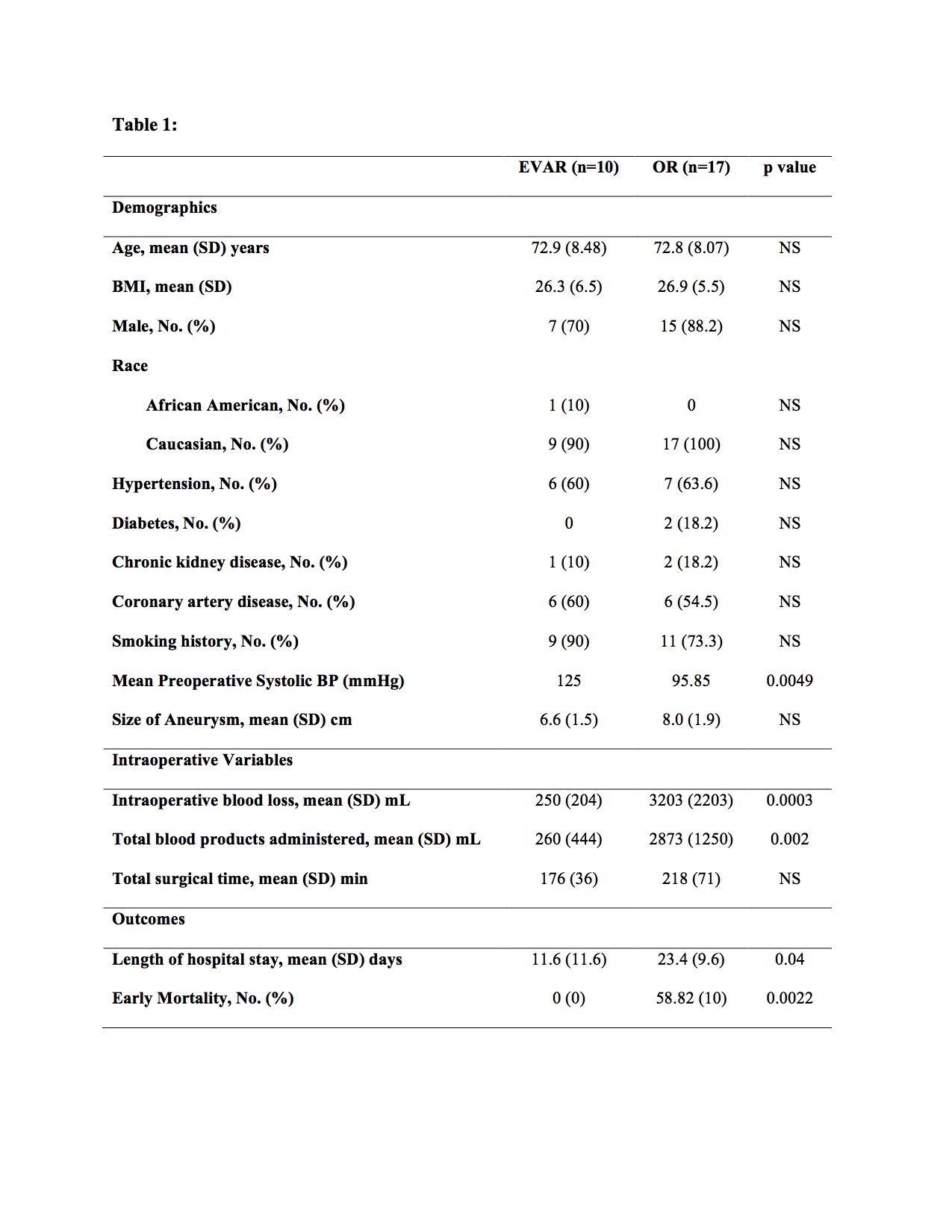
RESULTS: A total of 27 patients presented with rAAA. EVAR was done in 11 patients whereas 16 patients underwent open repair (OR). One patient with attempted EVAR was converted to open surgery. While there were no significant differences in the demographics and surgical time between the two groups, the EVAR group had significantly reduced mortality, blood loss, use of blood products, and postoperative complications. (Table 1) A classification table based on logistic regression showed that in predicting 30 day mortality status, the logistic model classified EVAR 100% correctly and OR 59% correctly with an overall 74% correct predictive rate for both procedures.
CONCLUSIONS: At our institution we observed that for the treatment of rAAA, EVAR was superior to OR with significant reduction in mortality and morbidity rates and length of hospital stay. Our results indicate that dedicated vascular teams using advanced endovascular techniques can enable EVAR to be performed emergently even on hemodynamically unstable patients with improved outcomes for rAAA patients as compared to OR. 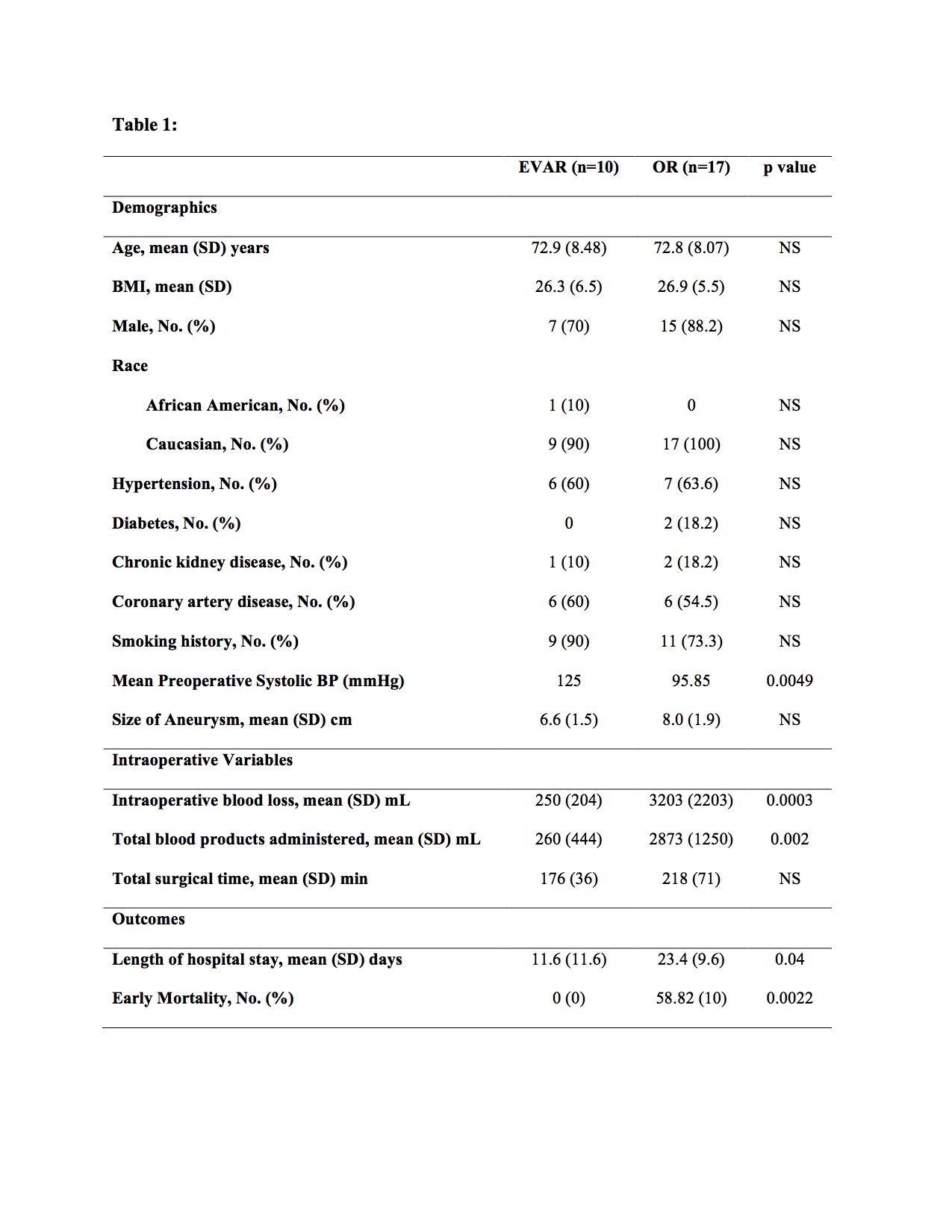
Back to 2016 Annual Symposium ePosters
|