|
Back to 2016 Annual Symposium ePosters
Socioeconomic status is a predictor of readmission within a year after EVAR
Daniel J. Torrent, MD, Michael C. Stoner, M.D., Charles Steven Powell, M.D., Frank M. Parker, M.D., William M. Bogey, M.D., Mandy R. Maness, M.D., Jack Yazbeck, M.D., Dean J. Yamaguchi, M.D..
East Carolina University, Greenville, NC, USA.
OBJECTIVES:
Socioeconomic status (SES) has been linked to worse disease at presentation and outcomes in vascular disease. National database studies have evaluated readmission after abdominal aortic aneurysm (AAA) repair but this has not been studied using single institutional data. The purpose of our study was to evaluate risks for readmission in single institutional data and determine whether SES has in impact on risk of readmission.
METHODS:
A retrospective cohort of patients who underwent endovascular aneurysm repair (EVAR) over a twelve year period at our institution was assembled. Demographics, comorbidities, complications, median per capita income in the county of residence, and readmission within one year of operation were recorded. Three SES groups (HIGH, MIDDLE, LOW) were formed based on the highest, lowest, and middle two quartiles for median per capita income in county of residence. Correlations were assessed using univariate statistics and a Cox model was constructed using backward selection.
RESULTS:
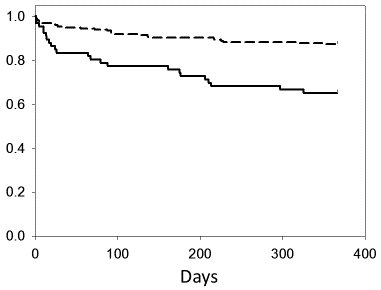
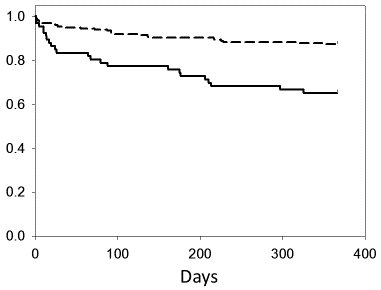
269 patients underwent EVAR with a total of 83,455 post-discharge days. The mean age was 74.3±0.5 years. There were 213 (79.2%) males and 228 (85.4%) were Caucasian. There were 48 readmissions (18.3%). Readmission after EVAR were associated with (p<0.05) LOW SES, complication, return to operating room, and post-operative infection during initial hospital stay. On Kaplan-Meier regression the MID SES and HIGH SES groups had similar rates of readmission and were subsequently grouped together. The LOW SES had significantly (p < 0.01) higher rates of readmission on a curve when compared to the MID and HIGH SES groups individually or the MID and HIGH SES groups combined (Figure 1). On Cox Regression LOW SES was associated (RR = 3.27, p<0.001) with increased risk of readmission in a model that also included complications (RR = 3.82, p = 0.03) and return to OR (RR = 3.78, p = 0.05). Infection was not significant when these other factors were in the model.
CONCLUSIONS:
In the largest single institution cohort, post-operative complications are associated with readmission which is similar to results seen in multi-institutional data. Additionally, LOW SES is a strong independent predictor of readmission after EVAR.
Figure 1. Time to readmission in days for HIGH/MID SES group (dashed line) compared to LOW SES group (solid line) after discharge for EVAR (p < 0.001).
Back to 2016 Annual Symposium ePosters
|