Back to 2016 Annual Symposium ePosters
Novel Intraoperative Neurophysiologic Monitoring Techniques during Thoracic Endovascular Aortic Repair (TEVAR) to Rapidly Assess Central Spinal Cord versus Peripheral Limb Ischemia
Leslie H. Lee, MD, Jason T. Lee, MD, Eric D. Jones, CNIM, Kenneth Eichenbaum, MD, Jaime R. López, MD.
Stanford University School of Medicine, Stanford, CA, USA.
OBJECTIVE: The utility of intraoperative neurophysiologic monitoring (IONM), including somatosensory evoked potentials (SSEPs) and/or transcranial motor evoked potentials (tcMEPs) during TEVAR has previously been described, but there remains no consensus regarding standardized neuromonitoring protocols. Traditional SSEPs and tcMEPs alone may not adequately distinguish potential central spinal cord versus peripheral limb ischemia, which is of critical importance, as treatment interventions may differ significantly in each scenario. We present a novel multimodality IONM approach to facilitate rapid assessment and prompt differentiation of contributing factors to suspected ischemia.
METHODS: We present two TEVAR cases for which a unique multimodality IONM protocol was employed that incorporates pudendal and perianal SSEPs, anal sphincter tcMEPs, the traditional use of upper and lower extremity SSEPs and tcMEPs, as well as electroencephalography (EEG).
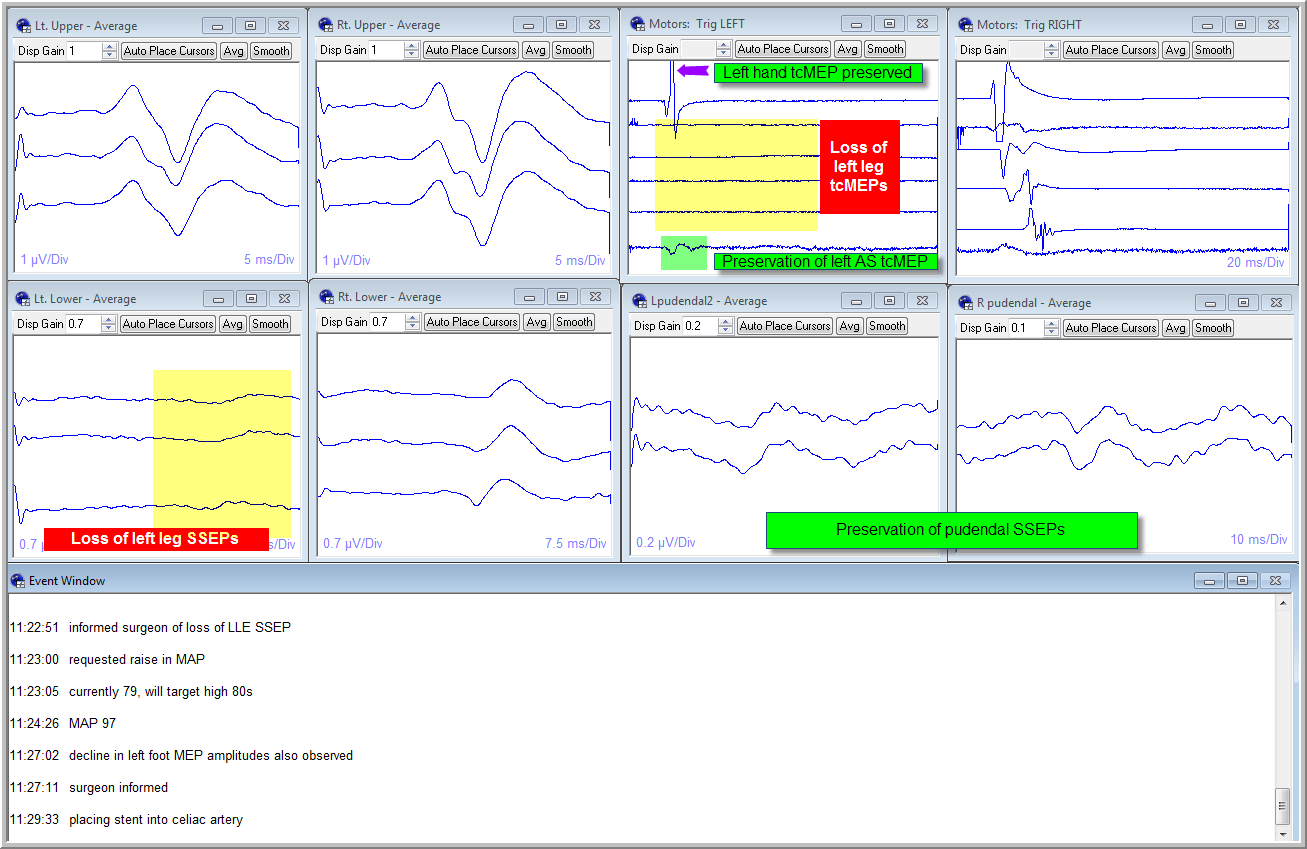
RESULTS: In both cases reproducible pudendal/perianal SSEPs and anal sphincter tcMEPs were obtained at baseline. During one case, sudden loss of left lower extremity SSEPs and tcMEPs was observed following sheath placement for selective vessel catheterization. In contrast, anal sphincter tcMEPs and pudendal/perianal SSEPs remained unchanged. This pattern was consistent with transient peripheral limb ischemia rather than spinal cord ischemia (SCI). As a result, mild blood pressure augmentation was instituted without a need for more aggressive interventions such as lumbar CSF drainage. Following stent deployment and sheath removal the left lower extremity SSEPs and tcMEPs returned to baseline and were stable through the end of case. In the second case, no changes were observed in any IONM modality. Both patients awoke postoperatively with no new neurologic deficits or new bowel/bladder symptoms to suggest recent or delayed SCI. 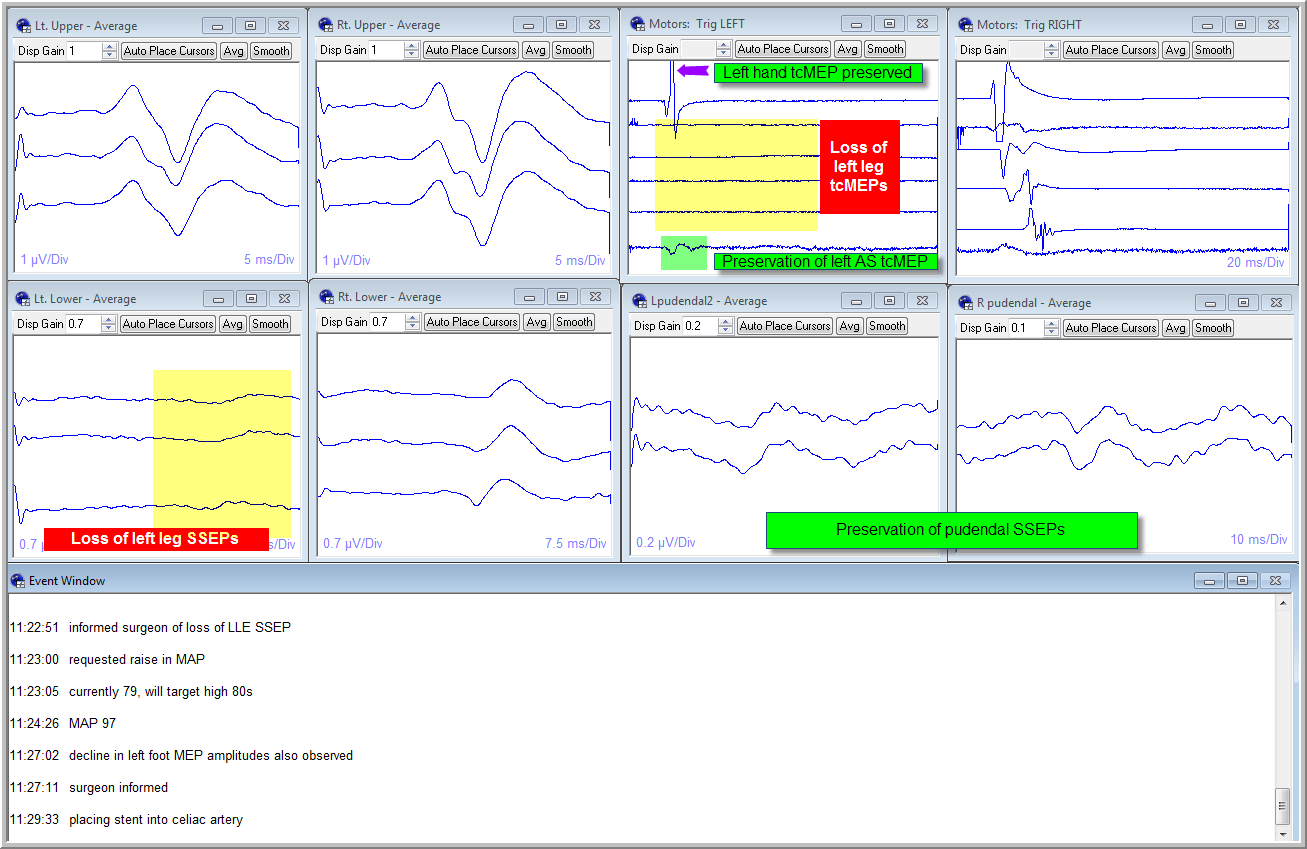
CONCLUSIONS: Spinal cord and limb ischemia are potential complications of TEVAR. The loss of extremity SSEPs/tcMEPs with preservation of pudendal/perianal SSEPs and anal sphincter tcMEPs suggests peripheral limb ischemia rather than SCI. We advocate the routine monitoring of pudendal/perianal SSEPs and anal sphincter tcMEPs, in conjunction with traditional IONM techniques, to allow for rapid differentiation between central and peripheral causes of evolving ischemia. The surgeon may then better ascertain the need for more aggressive versus conservative treatment interventions with the goal of optimizing perioperative and postoperative functional outcomes.
Back to 2016 Annual Symposium ePosters
|