Back to 2016 Annual Symposium ePosters
Redo Carotid Endarterectomy Versus Stenting: Durability and Midterm Outcomes
Isibor Arhuidese, MD MPH, Tammam Obeid, MD, Besma Nejim, MD, Mahmoud Malas, MD MS.
Johns Hopkins Medical Institutions, Baltimore, MD, USA.
Introduction: Re-stenotic carotid artery lesions are biologically different from de novo lesions. Although those lesions are less likely to cause a stroke but when they are critical or symptomatic they represent a treatment challenge. In this study, we perform a population based evaluation of carotid endarterectomy (CEA) vs carotid artery stenting (CAS) outcomes in a large cohort of patients who underwent prior ipsilateral CEA.
Methods: We studied all patients in the Vascular Quality Initiative (VQI) database, who underwent CEA or CAS after prior ipsilateral carotid revascularization between January 2003 and April, 2015. Univariate methods (Chi Square, ttest), multivariate logistic, cox regression and log rank tests were employed to compare patients’ characteristics and outcomes within 30days and in the mid-term.
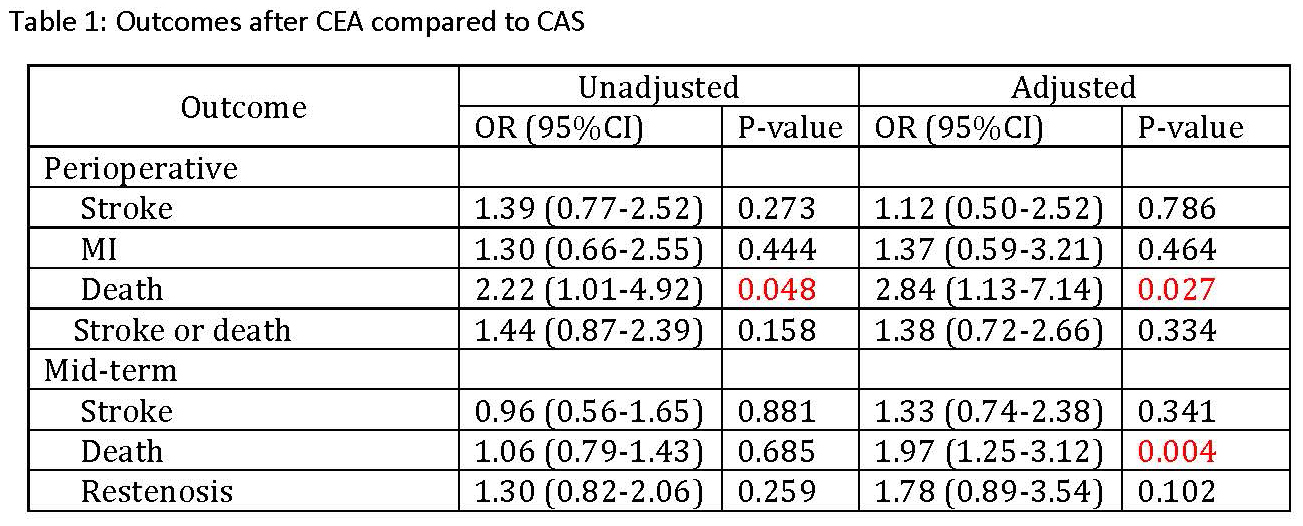
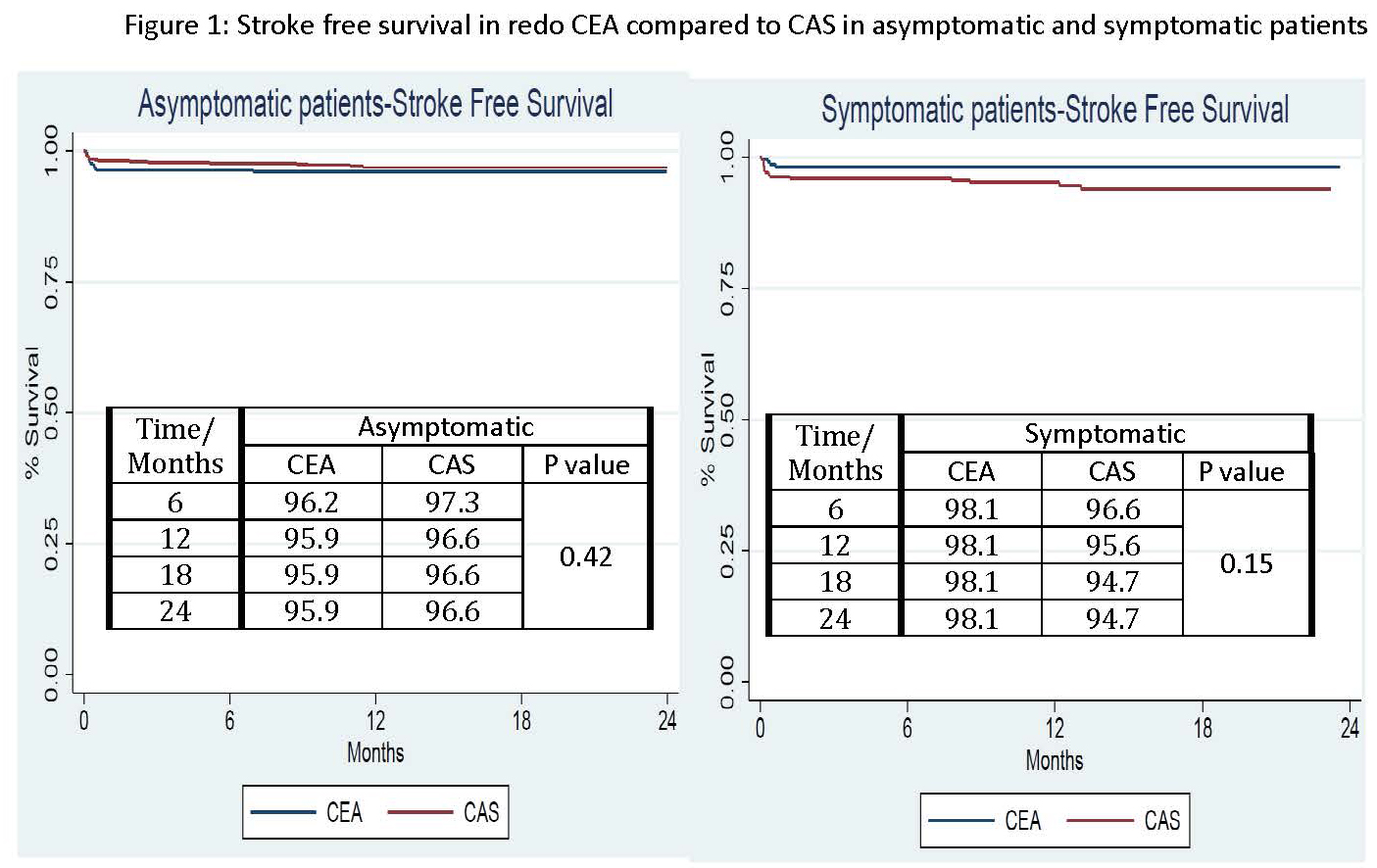
Results: There were 2863 carotid interventions (CEA: 1047-37%; CAS: 1816-63%) performed. The patients who underwent CEA vs CAS had similar age, gender, race and comorbidities. Perioperative ipsilateral stroke rate comparing CEA vs CAS was 2.2% vs 1.3% (p=0.09) for asymptomatics and 1.2% vs 1.6% (p=0.604) for symptomatic patients. Perioperative mortality and myocardial infarction after CEA vs CAS was 1.3% vs 0.6% (p=0.04) and 1.4% vs 1.1% (p=0.443), respectively. Cranial nerve injury occurred in 2.5% of the redo-CEA cases. CEA was associated with an increased risk of death at 30 days and in the mid-term (table 1). However, there were no differences in stroke, MI and restenosis between CEA and CAS after adjusting for patient characteristics. Stroke free survival was also similar between groups (Figures 1). The significant predictors of stroke or death were: increasing age (OR: 1.06, 95%CI: 1.03-1.09, p<0.001) and CHF (OR: 1.71, 95%CI: 1.02-2.86, p=0.040).
Conclusions: To our knowledge this is the largest study to date to evaluate midterm outcomes of carotid revascularization in patients with prior ipsilateral CEA. Redo carotid endarterectomy is associated with increased mortality and cranial nerve injury compared to CAS. Although, most restenotic lesions are benign, CAS is a safer revascularization approach when the need to intervene arises. 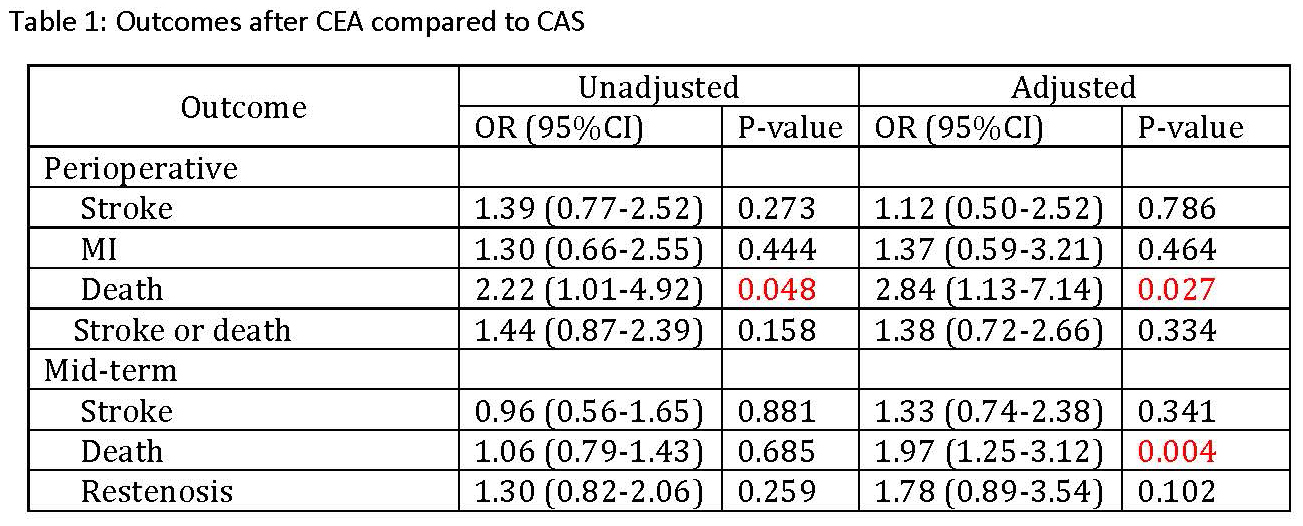 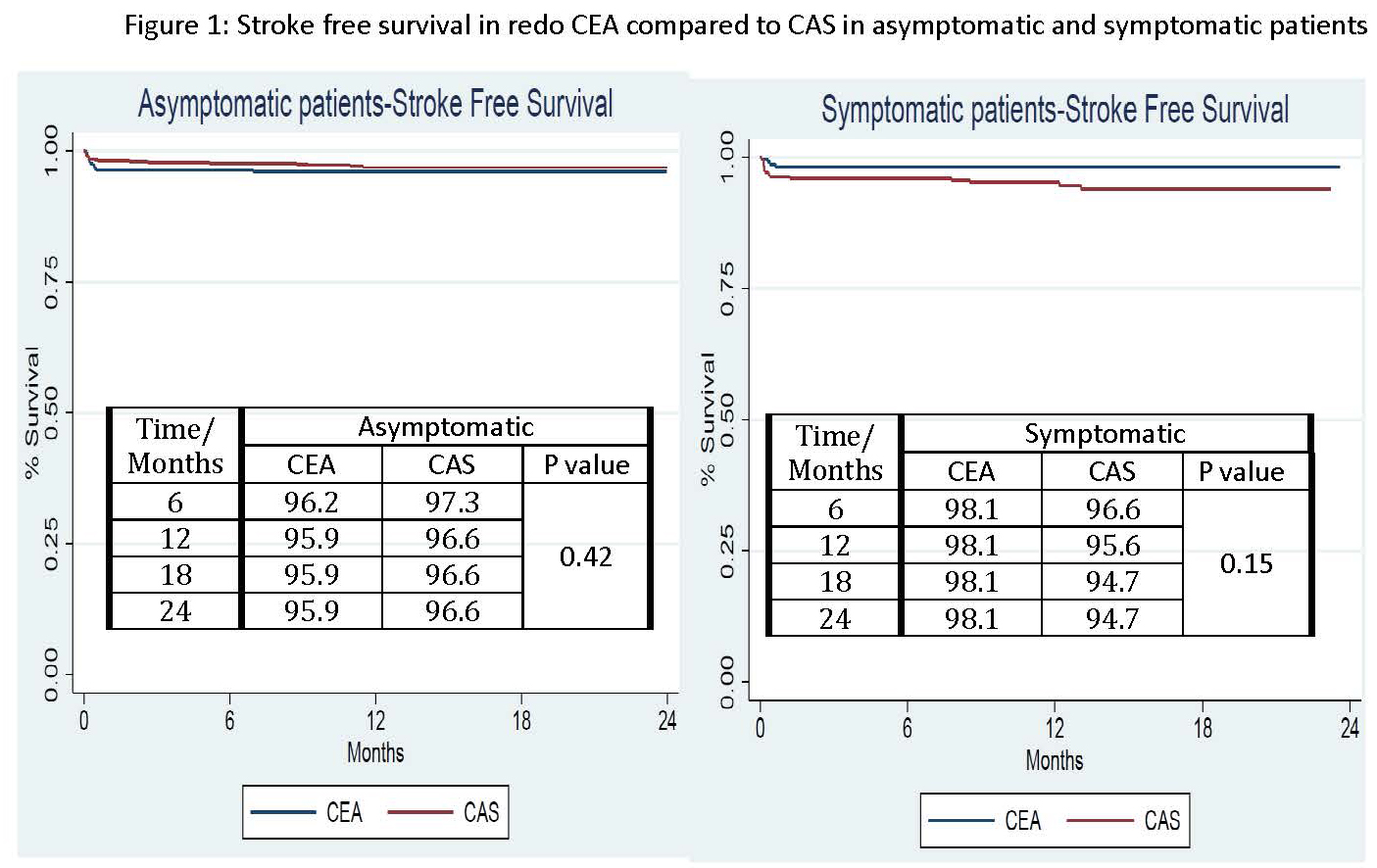
Back to 2016 Annual Symposium ePosters
|