Utilization of Intravascular Ultrasound to Assess Vascular Invasion in Pancreatic Cancer Post Chemoradiation Therapy
Anthony Feghali, MD, Kwame Amankwah, MD.
SUNY Upstate Medical University, Syracuse, NY, USA.
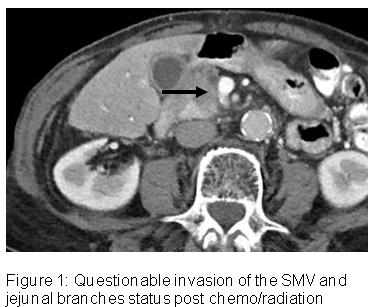
Objectives: Describe an intravascular ultrasound strategy as an adjunct modality in assessing tumor vascular invasion. Methods: An 80-year female presented with a one-month history of back pain. Work-up revealed a hypoechoic mass in the head of the pancreas with ERCP biopsy confirming pancreatic adenocarcinoma. A CT demonstrated the pancreatic mass abutting the SMV near its confluence with the splenic vein. No vascular invasion noted and patient considered a surgical candidate.
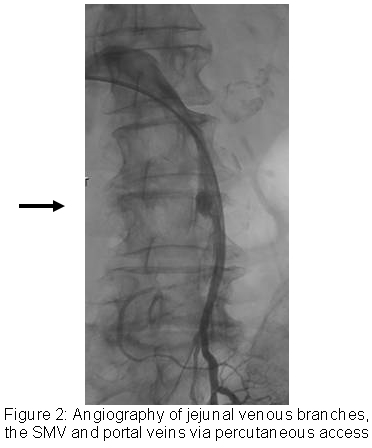
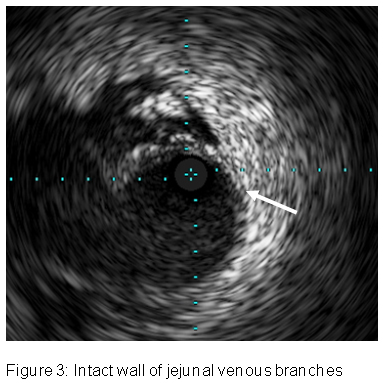
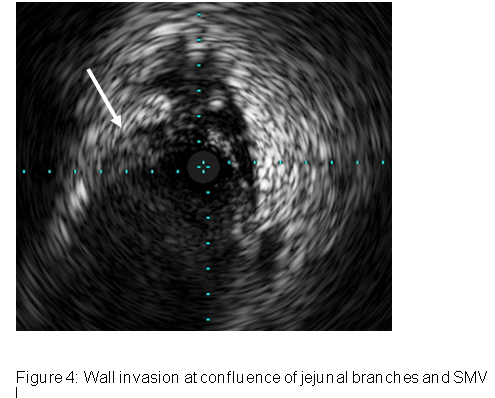
The patient did not want surgery and underwent chemoradation but after 3 months wanted surgery. The mass decreased in size; however, there was progressive involvement of the fat plane of jejunal branches as they become the SMV. Vascular involvement could not be excluded (Figure 1). Patient underwent a percutaneous transhepatic intravascular ultrasound (IVUS) of the portal system to evaluate for tumor extension into the vessels. The right portal vein was accessed and a venography was performed to delineate the SMV, jejunal venous branches and splenic vein (Figure 2). A 5 French intravascular ultrasound (IVUS) probe (Eagle Eye) was advanced and images were obtained with fluoroscopy (Figures 2-4).
Results: There was complete obliteration of the echogenic wall of the jejunal branch at convergence with SMV. At least a 0.5 cm distal cuff of SMV is needed for anastomosis thus the patient was not considered a surgical candidate. Conclusions: CT is the primary modality to assess tumor involvement with vasculature for resectability. However, CT and other non-invasive imaging cannot differentiate between vascular invasion and compression. IVUS represents a modality that can delineate vascular involvement. This case represents a first report of IVUS used post chemoradiation to determine a patient's candidacy for resection.
Back to 2017 ePosters




