Increasing Use of Endovascular Therapy in Pediatric Vascular Trauma
Bernardino C. Branco, MD, Bindi Naik-Mathuria, MD, Miguel Montero-Baker, MD, Ramyar Gilani, MD, Charles A. West, MD, Joseph L. Mills, MD, Jayer Chung, MD, MSc.
Baylor College of Medicine, Houston, TX, USA.
Background: Little is known regarding the epidemiology and outcomes of endovascular treatment of pediatric vascular injuries (ePVI). We evaluated recent trends in ePVI, and its association with early survival.
Methods: An 8-year analysis of the National Trauma Databank (2007-2014) was performed to extract children (age ≤16 years) with vascular injuries. Demographics, vitals, injury severity score (ISS), interventions and mortality were obtained. χ2, Kruskall-Wallis, Cochrane-Armitage and logistic regression were used where appropriate.
Results: Among 2,504,213 traumas, there were 35,771 (1.4%) patients with vascular injuries, 3,637 of whom were children (10.1% of all vascular injuries). Of these, 2,179 patients (72.2% male; mean age 10.6 + 4.8 years) underwent 2,518 therapeutic vascular procedures (263 [10.4%] endovascular; 2,255 [89.6%] open). ePVI was utilized in 219 blunt (83.3%) , 28 (10.6%) penetrating and 16 (6.1%) injuries of unknown mechanism (p < 0.001). The percentage of ePVI increased (from 7.8% in 2007 to 12.9% in 2014, p=0.04; Figure 1), with a corresponding increase in ePVI with ISS (p < 0.001) or age (p < 0.001). Concomitantly, the proportion of in-hospital deaths after vascular procedures decreased (from 6.5% in 2007 to 2.3% in 2014; p=0.01). The most common endovascular procedures performed were unspecified aneurysm repair (187, 71%), insertion of a stent (26, 9.8%) and thoracic aortic endograft placement (16, 6.1%). There were 331 decedents (9.1% of PVI). Decedents had a significantly higher ISS (p < 0.001), and more penetrating injuries (39.9% versus 31.1%; p = 0.04). Between endovascular and open procedures, in-hospital mortality did not differ (1.2% vs. 1.8%, p=0.73). Multivariable logistic regression identified lack of signs of life on arrival (OR 10.6 [95% CI: 7.3-13.7]; p<0.001), GCS≤8 (OR 1.7 [1.1-2.3]; p<0.001), ISS≥16 (OR 4.0 [3.0-5.2]; p<0.001), positive ethanol/drug screen on admission (OR 2.3 [1.1-5.2]; p=0.04) and SBP<90 mm Hg (OR 4.3 [3.2-5.9]; p<0.001) as independent predictors for death.
Conclusions: While uncommon, almost 10% of children with vascular injuries die during their initial admission. ePVI is being utilized more frequently despite the lack of robust outcomes data, or devices designed for children. Long-term, multicenter, prospective registries are required to determine the appropriate applications of ePVI. 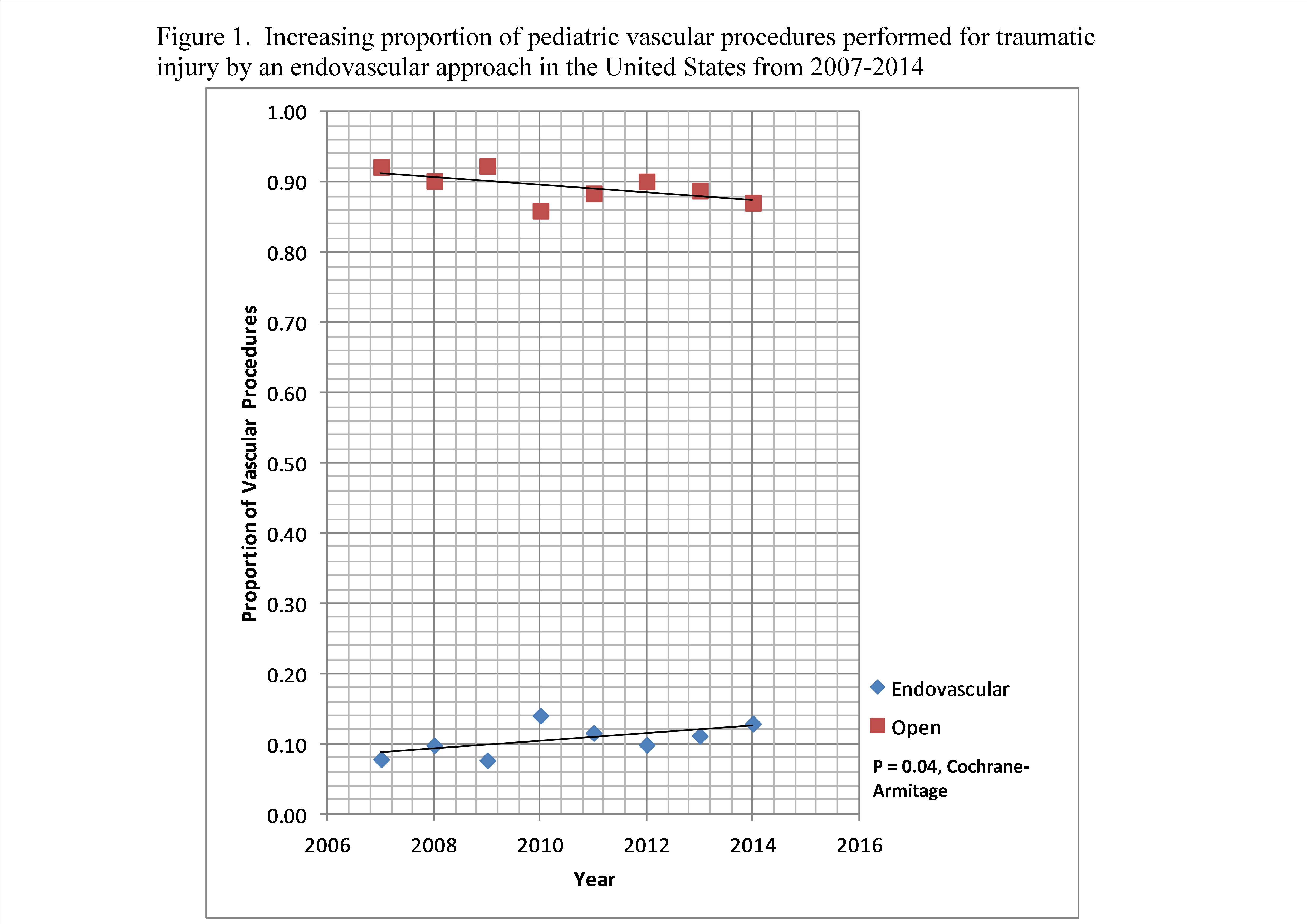
Back to 2017 ePosters




