Carotid Artery Revascularization in Patients with Contralateral Carotid Artery Occlusion: Stent or Endarterectomy?
Besma J. Nejim, MBChB, MPH, Satinderjit Locham, MD, Hanaa Dakour Aridi, MD, Caitlin W. Hicks, MD, MS, Mahmoud B. Malas, MD, MHS.
Johns Hopkins Medical Institutions, Baltimore, MD, USA.
Objective: The Center for Medicare and Medicaid Services (CMS) considers carotid endarterectomy (CEA) a high risk procedure for patients with contralateral carotid artery occlusion and agrees to reimburse for carotid artery stenting (CAS). However, there is paucity of evidence that support the superiority or the equipoise of CAS compared to CEA in this patient population.
Methods: All patients who underwent CEA or CAS with contralateral occlusion were identified in the Vascular Quality Initiative registry between 2005 and 2016. Outcomes examined were stroke, death and MI at 30 days and stroke and death at 2 years. Multivariable logistic regression analysis controlling for potential confounders as well as life tables, robust Cox proportional hazard and log rank tests were used.
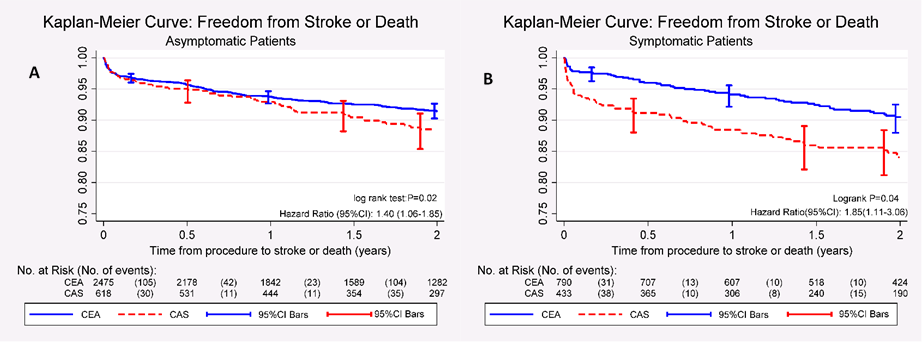
Results: Overall, 4,326 patients had contralateral occlusion [CEA: 3,274 (75.7%) versus CAS: 1,052 (24.3%)]. In general, patients' demographics and comorbidities were similar in both groups, except for black race and history of congestive heart failure which were more prevalent in the CAS group (9.5% vs. 7.6%; P=.048) and (15.6% vs. 9.6%; P<.001) respectively, while history of previous stroke was more prevalent in patients undergoing CEA (56.4% vs. 24.0%; P<.001). CAS patients were more likely to present with ipsilateral symptoms (41.2% vs. 24.2%; P<.05). The 30-day stroke death and MI didn't differ between the two procedures in asymptomatic patients yet in symptomatic patients, CAS was associated with almost threefold higher stroke risk and over fourfold mortality [OR (95%CI): 2.77 (1.07-7.21), P=.036] and [OR (95%CI): 4.61(1.63-13.03), P=.004] respectively. The 2-year risk of any stroke/death was 40% higher with CAS in asymptomatic patients [adjusted hazard ratio (95%CI): 1.40 (1.06-1.85); P=.02], while, it was 85% higher with CAS in symptomatic patients [aHR (95%CI): 1.85 (1.11-3.06); P=0.02] (Figure)
Conclusion: CAS is not safer than CEA in patients with contralateral carotid artery occlusion. In the perioperative period, CAS performance was similar to CEA in asymptomatic patients and had significantly worse outcomes in symptomatic patients. The two-year risk of stroke or death was consistently higher for CAS. Refinement of current guidelines is warranted to provide surgical care specifically tailored for patient's characteristics and clinical presentation.
Back to 2017 ePosters




