TEVAR for a patient with intramural hematoma after failure of medical therapy
Harleen K. Sandhu, MD, Samuel Leonard, BS, Samuel Leake, BS, Wande Pratt, MD, MPH, Ali Azizzadeh, MD.
University of Texas Medical School at Houston, Houston, TX, USA.
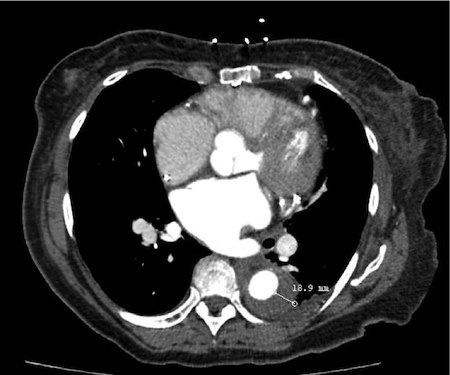
OBJECTIVES: Patients with uncomplicated classic Type B aortic dissections are typically managed with antiimpulse control (SBP <120 mm Hg, heart rate <60 bpm) and pain management. However, there are currently no established guidelines for treatment of isolated intramural hematoma (IMH) of the descending aorta. IMH is defined as hemorrhage into the arterial media (intimomedial plane) without an intimal flap. IMH represents 1% of acute aortic syndromes and diagnosis can be difficult as presentation is often indistinguishable from thrombosed classic Type B aortic dissection with intimal flap healing. We present a case of endovascular intervention for a patient with IMH who showed persistent intractable pain and progression. METHODS: A 74 year-old African American woman with a past medical history of hypertension, atrial fibrillation, diabetes mellitus, coronary artery bypass grafting, and automatic implantable cardioverter-defibrillator presented to an outside hospital after developing anterior chest and back pain. Contrast-enhanced computed tomography (CTA) on admission revealed a proximal thoracic aortic IMH (figure 1) extending to the celiac artery. RESULTS: We managed the patient medically with antiimpulse control. Despite medical therapy the patient continued to experience persistent, intractable pain. Repeat CTA demonstrated IMH growth (figure 2). On hospital day 10, the patient was treated with thoracic endovascular aortic repair without coverage of the left subclavian artery. Intravascular ultrasound was used to assess proximal and distal landing zones, true lumen reexpansion, and branch vessel patency. At one month followup clinic visit she is recovering uneventfully with a decreased level of pain. CONCLUSIONS: This case illustrates the dynamic pathology of descending thoracic aortic IMH. Thoracic endovascular repair is a suitable option for patients that fail medical therapy. Intravascular ultrasound is a useful adjunct in determining extent of aortic coverage, assessing proximal and distal landing zones, and identifying true lumen re expansion. Treatment of patients with uncomplicated IMH in the descending aorta remains at the discretion of the treating physician. Further studies are needed to ascertain optimal management. 
Back to 2017 ePosters




