Differences in Predictors of Intraoperative versus Postoperative Strokes after Carotid Endarterectomy and Carotid Artery Stenting.
Alexander B. Pothof, MD MS1, Thomas F. O'Donnell, MD1, Gert J. de Borst, MD2, Marc L. Schermerhorn, MD1.
1BIDMC, Boston, MA, USA, 2UMC Utrecht, Utrecht, Netherlands.
OBJECTIVES: Pathophysiological mechanisms of intra-operative strokes differ from post-operative strokes. Carotid stent (CAS) patients more often experience an intraoperative stroke compared to carotid endarterectomy (CEA) patients. However, our understanding of differences in predictors of intraoperative strokes between patients undergoing CEA and CAS is limited.
METHODS: We identified CEA and CAS patients in the VQI registry (2012-2017) and excluded patients missing data on symptom status (N=341), ipsilateral occluded internal carotid artery (ICA) (N=1950), concurrent cardiac surgery (N=1139), concurrent carotid bypass (N=750), and emergency cases (N=993). After stratification on treatment modality, we used multilevel logistic regression to identify predictors for intraoperative, early (<6 hours), and late (>6 hours) postoperative in-hospital strokes.
RESULTS: We included 61,934 CEA (43,404 (70%) asymptomatic), and 11,703 CAS patients (6911 (59%) asymptomatic). Among CEA patients, stroke rate was 1.0% (N=615), with 93 (15%) intraoperative, 285 (47%) early, and 235 (38%) late postoperative strokes. Among CAS patients, stroke rate was 1.9% (N=228), with 51 (23%) intraoperative, 92 (41%) early, and 84 (37%) late postoperative strokes. For CEA patients, intraoperative, compared to early or late postoperative strokes, had a higher median modified Rankin Scale, with 4.(IQR:2-4) vs. 3.(IQR:2-4), P=.01); vs. 2.5.(IQR:1-4), P=.004), whereas stroke severity was comparable between strokes in CAS patients (P>.05).
Among CEA patients, preprocedural ipsilateral stroke was predictive for any stroke. The independent predictors for intraoperative strokes were concomitant angioplasty/stent of the more distal ICA or bifurcation and ipsilateral ICA stenosis ≤70% (Table 1), whereas CEA with patch was protective. Among CAS patients, the independent predictors for intraoperative strokes were admission from a nursing home, Hispanic ethnicity, and receiving multiple stents. Moreover, after adjustment, including CMS high risk criteria, CAS was associated with higher risk of intraoperative stroke (OR:2.6 [1.6-4.2] P < .001) compared to CEA.
CONCLUSION: The differences in risk factors between CEA and CAS for intraoperative strokes illustrate opportunities for quality improvement efforts. These are of paramount importance for CAS patients, who are at a higher risk for intraoperative strokes. 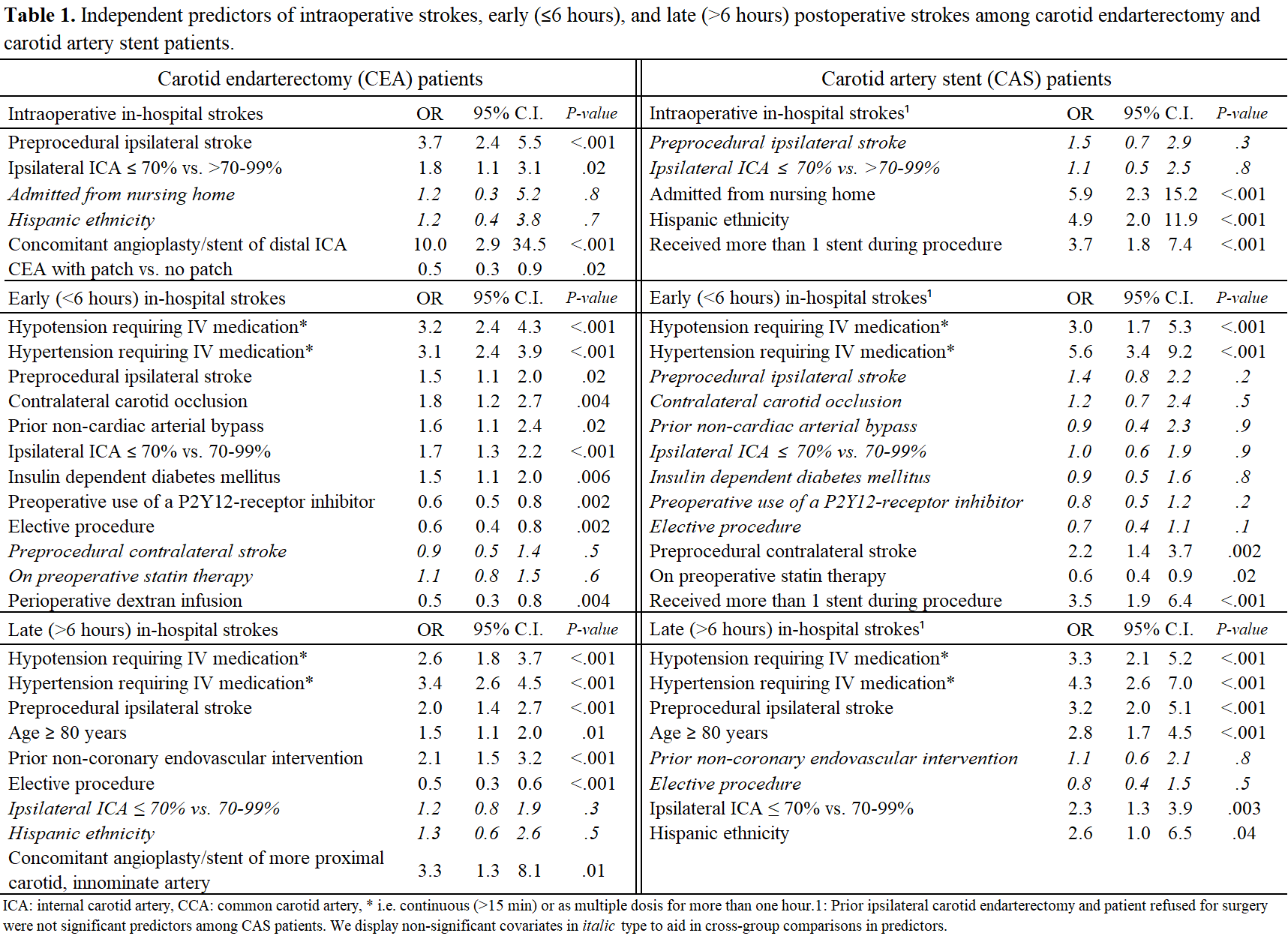
Back to 2018 Program




