Superior Mesenteric and Celiac Arteries Stenting does not Increase Complications Rate after F/BEVAR Endovascular Aortic Repair
Fernando Motta, MD, Corey A. Kalbaugh, PhD, MS, Jason Crowner, MD, Luigi Pascarella, MD, Katharine L. McGinigle, MD, William A. Marston, MD, Melina R. Kibbe, MD, Mark A. Farber, MD.
University of North Carolina, Chapel Hill, NC, USA.
Objective: Extension of complex endovascular aortic repair into the mesenteric arteries (Superior Mesenteric Artery[SMA] and Celiac Artery[CA]) may be associated with increased complications. The purpose of this study was to evaluate complications in patients undergoing complex endovascular aortic repair with ZFEN devices and those in a PSIDE clinical trial in order to compare groups defined by stenting location and the length of coverage above the celiac artery(CA).
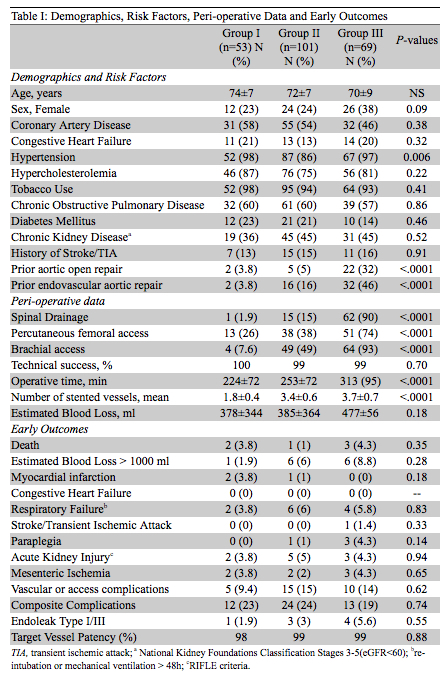
Methods: A retrospective review of a prospectively maintained database was performed on patients undergoing F/BEVAR procedures for thoracoabdominal aortic aneurysms between September 2012 and May 2017. Patients were grouped according to presence of stents in the SMA/CA and the length of aortic coverage above the CA: Group I (no SMA/CA stent), Group II (SMA/CA stent and <5 cm coverage above CA) and Group III (SMA/CA stent and >5 cm coverage above CA). Variables included demographics, risk factors, comorbidities, pre-operative aneurysms characteristics, procedural data, and early outcomes. Individual and composite complications were compared between groups (death, MI, respiratory failure, stroke/TIA, paraplegia, AKI, mesenteric ischemia and vascular complications).
Results: We treated 223 patients during the study period (mean age: 72 years; 76% male). There was no difference in demographics, risk factors and comorbidities between Groups, except hypertension was less common in Group II and history of previous aortic surgery was more common in Group III (Table I). Group II (15%) and III (90%) had higher spinal drain usage than Group I (2%; p<0.0001). Operative time and brachial access utilization were greater in Groups II and III compared with Group I (p<0.0001). There was no difference in technical success and mortality rates. Major complications (individually and composite analysis) were similar among groups. The 30-day CTA showed no difference regarding type I/III endoleaks and branch patency for Groups I, II and III, respectively (Table I).
Conclusion: Patients who needed SMA/CA incorporation with stents during F/BEVAR for aortic repair had more complex procedures, as assessed by operative time, brachial access, number of vessel incorporated and spinal drainage use. However, the extension of the repair did not impact the outcomes, demonstrated by similar mortality and complication rates between groups.
Back to 2018 Program




