Association of Aneurysm Sac Behavior with Long-Term Survival Following EVAR
Thomas FX O'Donnell, MD1, Sarah E. Deery, MD, MPH2, Jeffrey J. Siracuse, MD3, Marc L. Schermerhorn, MD1, Salvatore T. Scali, MD4, Andres Schanzer, MD5, Robert T. Lancaster, MD, MPH2, Virendra I. Patel, MD, MPH6.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Massachusetts General Hospital, Boston, MA, USA, 3Boston Medical Center, Boston, MA, USA, 4University of Florida Health, Gainesville, FL, USA, 5University of Massachusetts Medical Center, Worcester, MA, USA, 6New York Presbyterian/Columbia University Medical Center, New York, NY, USA.
OBJECTIVES: EVAR is associated with an early survival advantage over open repair, however that advantage reverses over time. This may result from the higher rates of reintervention related to endoleaks and aneurysm sac expansion. We thus undertook to examine the association between sac behavior, endoleaks, reintervention and long-term survival.
METHODS: We studied all patients undergoing EVAR in the Vascular Quality Initiative (VQI) between 2003 and 2017 with at least one follow-up imaging study. We defined aneurysm sac changes by SVS guidelines (change ≥ 5mm), and determined independent predictors of sac behavior, new endoleak, and reintervention using multivariable logistic regression. We employed Cox regression to examine the association between sac behavior and long-term survival.
RESULTS: Of 20,515 EVAR patients, 14,827 (72%) fit our criteria. In follow-up; 7,162 (48%) sacs remained stable; 6,574 (44%) regressed; and 1,091 (7%) expanded. Factors associated with sac expansion included age (by year: OR 1.02 [1.01-1.03], P<.01), aortic diameter (OR 2.49 [2.02-3.07], P<.01 for the smallest quintile), preoperative anemia (OR 1.38 [1.02-1.87], P=.04), Type 1 endoleak on completion angiogram (OR 1.59 [1.14-2.20], P<.01), and iliac aneurysms (OR 1.38 [1.20-1.59], P<.01) while statin therapy at discharge (OR 0.84 [0.72-0.98], P=.02), and current smoking (OR 0.70 [0.57-0.87], P<.01) were protective. Sac changes were independently associated with the development of new endoleak (sac expansion: OR 1.58 [1.34-1.86], P<.01; sac regression: OR 0.35 [0.31-0.40], P<.01), and reintervention (sac expansion: OR 2.26 [1.82-2.82], P<.01; sac regression: OR 0.59 [0.49-0.71], P<.01). Risk-adjusted Cox regression (patient characteristics, reintervention, and endoleak on completion or in follow-up), showed sac behavior was independently associated with long-term mortality (sac expansion: HR 1.4 [1.1-1.8], P<.01; sac regression: HR 0.82 [0.7-0.95], P<.01). Undergoing reintervention failed to modify the association between sac behavior and mortality (P=.74). Even in patients without documented endoleaks, sac behavior remained associated with long-term mortality (sac expansion: HR 1.4 [1.03-1.8], P=.01; sac regression: HR 0.8 [0.7-0.95], P<.01).
CONCLUSIONS: Following EVAR, aneurysm sac behavior is associated with the development of new endoleaks, undergoing reintervention, and long-term mortality. The association between sac behavior and long-term mortality persisted even in patients without endoleaks, and was not modified by reintervention. 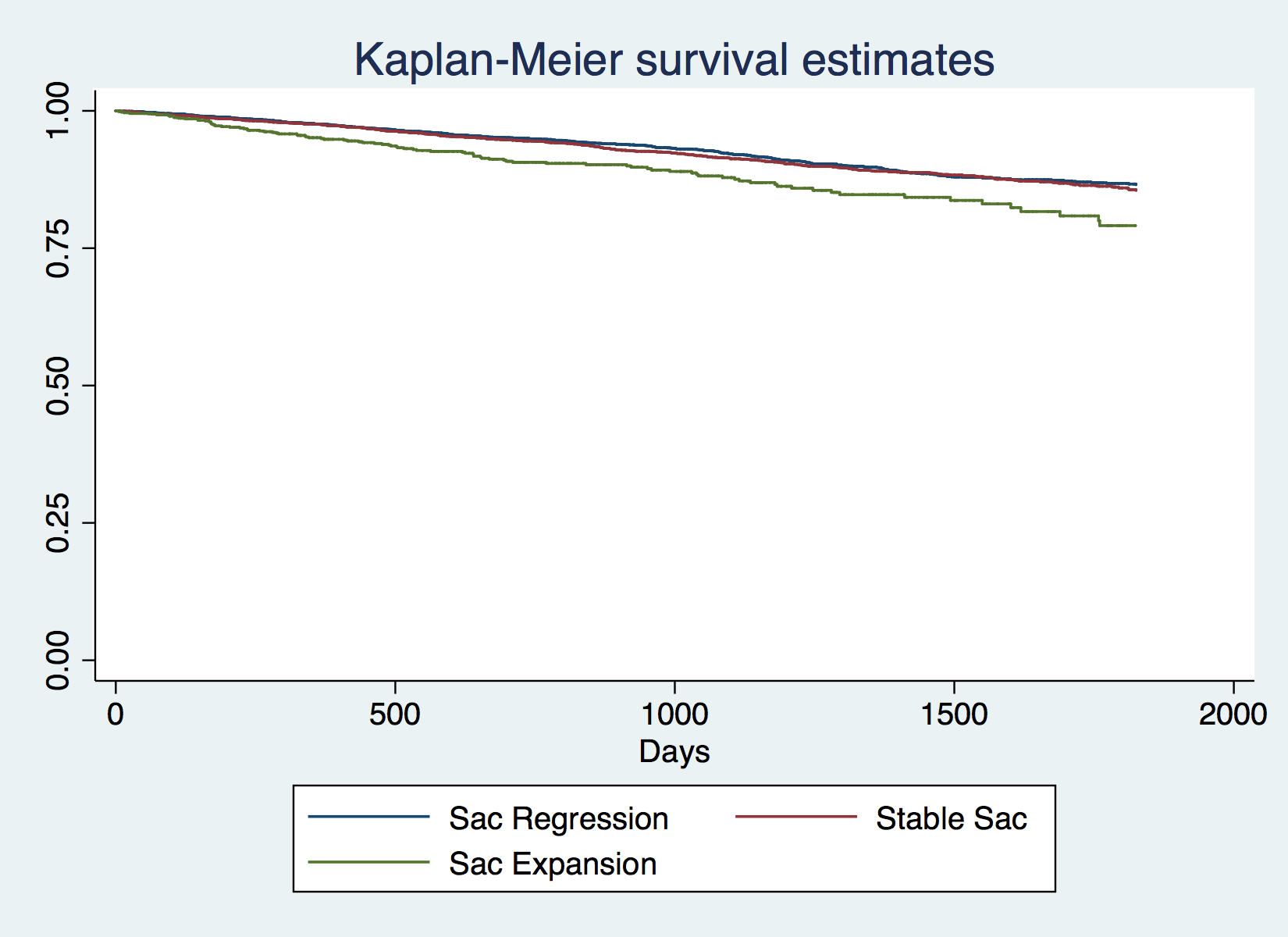
Back to 2018 Program




