Contemporary Outcomes of Thoracofemoral Bypass
Jeffrey Crawford, M.D., Salvatore T. Scali, M.D., Kristina A. Giles, M.D., Martin Back, M.D., M.S., Javairiah Fatima, M.D., Dean Arnaoutakis, M.D., Scott A. Berceli, M.D., Ph.D., Thomas S. Huber, M.D., Ph.D..
University of Florida-Gainesville, Gainesville, FL, USA.
Objectives: Thoracofemoral bypass (TFB) has been reported to be an alternative strategy to aorto-femoral (AFB) or extra-anatomic bypass for severe aorto-iliac occlusive disease (AIOD). TFB may be particularly useful in selected patients with concurrent visceral aortic branch vessel disease, infrarenal aortic occlusions or after failed aorto-femoral reconstruction. However, there is a paucity of data on TFB indications and outcomes with few contemporary series describing utility of the procedure. Therefore, the purpose of this analysis was to review our experience with TFB.Methods: All patients undergoing TFB for occlusive disease from 2002-2017 were reviewed. All subjects underwent left thoraco-retroperitoneal exposure of the supra-celiac aorta with division of the diaphragmatic crus and supra-celiac cross-clamping. An end-to-side aortic anastomosis was created and each graft limb was tunneled in the retroperitoneum to the femoral bifurcation. Adjunctive visceral or infra-inguinal revascularization was performed based on symptoms, end-organ function and/or preoperative imaging. The primary end-points were major complications and 30-day mortality. Secondary end-points included limb patency, freedom from major adverse limb events (MALE), and survival. Kaplan-Meier methodology was used to characterize end-points.Results: Forty-one patients [age: 61±9 years; female-54%, hypercoaguable state-7%] underwent TFB with perioperative features outlined in the Table. Mean preoperative ankle brachial index (ABI) was 0.4, bilaterally. Indications included: critical limb ischemia (56%), claudication (30%), acute limb ischemia (7%) and mesenteric ischemia (7%). Seven (17%) had previously undergone AFB. Adjunctive visceral bypass occurred in 8(20%) (14 grafts: renal-6, superior mesenteric artery-5, celiac-3). Postoperative LOS was 11[IQR 7, 16] days and 30-day mortality was 5%(n=2). Major complications occurred in 34% (n=14; pulmonary-15%, cardiac-12%, bleeding-7% [incidental splenectomy-5%], renal-5%, wound-2%). Mean postoperative ABI was 0.9, bilaterally.At median follow-up of 9.3[IQR 1, 17] months, 5(12%) patients underwent some form of re-intervention (graft/limb related-4[graft thrombosis-2, graft infection-2], mesenteric bypass revision-1). The 3-year primary limb patency, freedom from MALE and survival were 95±3%, 70±10%, and 93±4%, respectively. Conclusions: This experience represents the largest and most current series of TFB. We demonstrate that TFB can be performed with good outcomes for patients with severe AIOD, especially if concomitant visceral/infrainguinal reconstruction is warranted. These results support a continued role for TFB in selected patients. 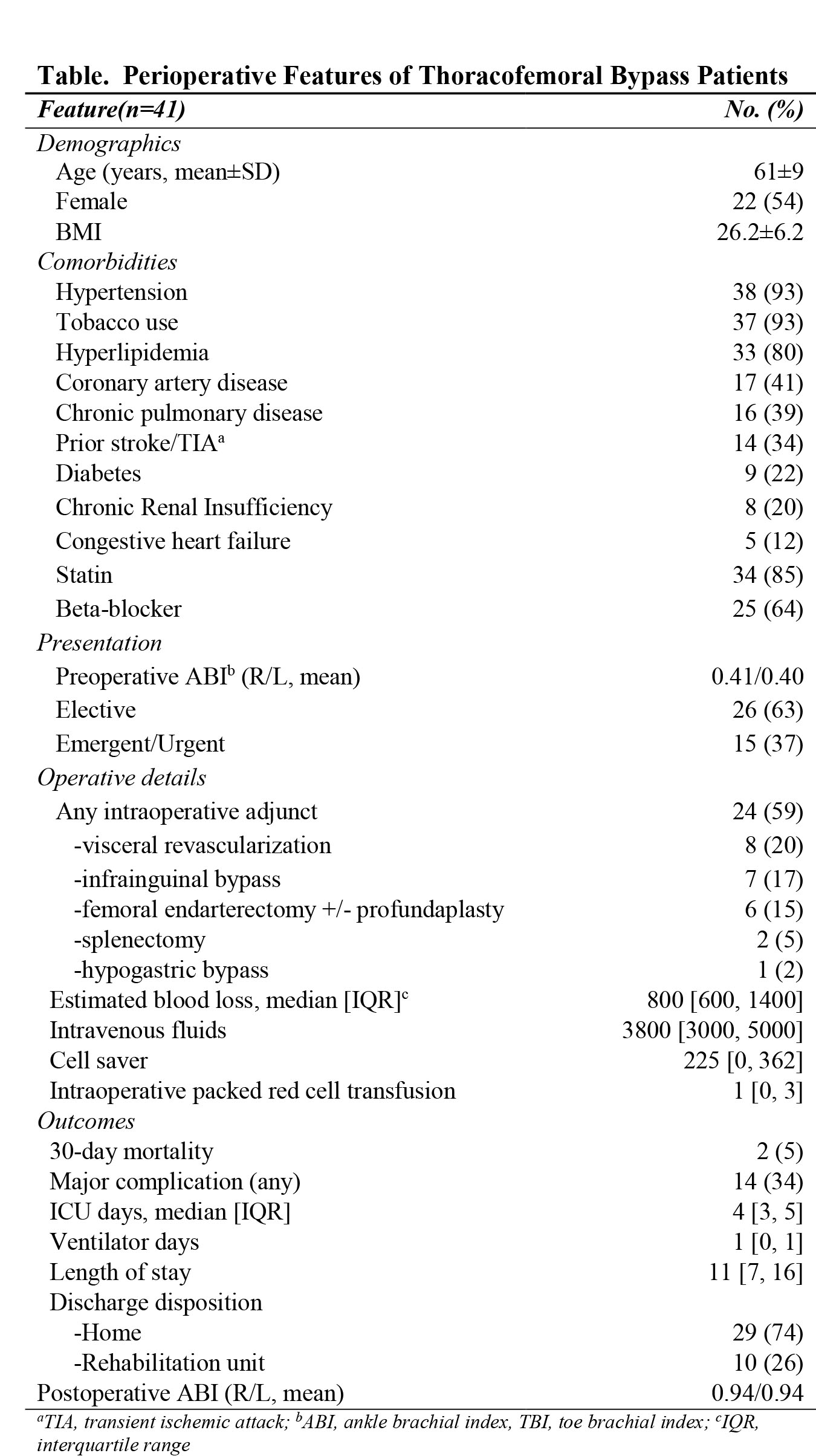
Back to 2018 Program




