Outcomes following first-time lower extremity revascularization for chronic limb-threatening ischemia in insulin-dependent diabetic patients
Jeremy D. Darling, M.S., Thomas F.X. O'Donnell, M.D., Sarah E. Deery, M.D., Anthony V. Norman, B.S., Giap H. Vu, B.A., Raul J. Guzman, M.D., Mark C. Wyers, M.D., Allen D. Hamdan, M.D., Marc L. Schermerhorn, M.D..
Beth Israel Deaconess Medical Center, Boston, MA, USA.
Objectives: Historically, open surgical bypass provided a durable repair among diabetic patients with chronic limb-threatening ischemia (CLTI). In the current endovascular era, however, the difference in long-term outcomes between first-time revascularization strategies among patients with insulin-dependent diabetes (IDDM) is poorly understood. Methods: We reviewed all patients with IDDM undergoing a first-time infrainguinal bypass (BPG) or percutaneous transluminal angioplasty (PTA/S) for CLTI at our institution from 2005-2014. We defined IDDM as insulin administration at baseline to control blood glucose levels. We compared rates of wound healing, restenosis, re-intervention, major amputation, and mortality between BPG and PTA/S using Chi-square, Kaplan-Meier, and Cox regression analyses. As a sensitivity analysis, we calculated propensity scores and employed inverse probability weighting to account for nonrandom assignment to BPG versus PTA/S. Results: Of 2,869 infrainguinal revascularizations from 2005-2014, 703 limbs (343 BPG, 361 PTA/S) in 682 patients fit our criteria. BPG patients, compared to PTA/S, were similar in age (69 vs. 68 years; P=.51), rates of tissue loss (87% vs. 91%; P=.055), and dialysis-dependence (25% vs. 28%; P=.34), were less likely to be hypertensive (84% vs. 93%; P<.01), and more likely to be current smokers (21% vs. 14%; P=.02). There were no differences between BPG and PTA/S in mean HbA1c levels (7.9 vs. 8.0; P=.52) or mean fasting blood glucose levels (152 vs. 156; P=.47). Perioperative complications did not differ, including acute kidney injury (20% vs. 23%; P=.26), hematoma (7.3% vs. 4.2%; P=.07), acute myocardial infarction (1.5% vs. 2.2%; P=.46), and mortality (3.8% vs. 2.8%; P=.45). Unadjusted 6-month rates of incomplete wound healing (51% vs. 59%) and 5-year rates of restenosis (48% vs. 64%) and re-intervention (49% vs. 60%) were all significantly higher after PTA/S (P<.05). After adjustment, multivariable analysis suggested PTA/S-first intervention to be significantly associated with higher risk of restenosis (Hazard Ratio (HR), 1.6; 95% Confidence Interval [1.1-2.4]) and re-intervention (2.0 [1.3-3.0]); these results remained robust following inverse probability weighting. Conclusion: Among patients with CLTI, insulin-dependent diabetes is associated with a high risk of adverse events. Ultimately, our data suggest that a bypass-first approach may best serve appropriately selected, anatomically suitable patients within this vulnerable population. 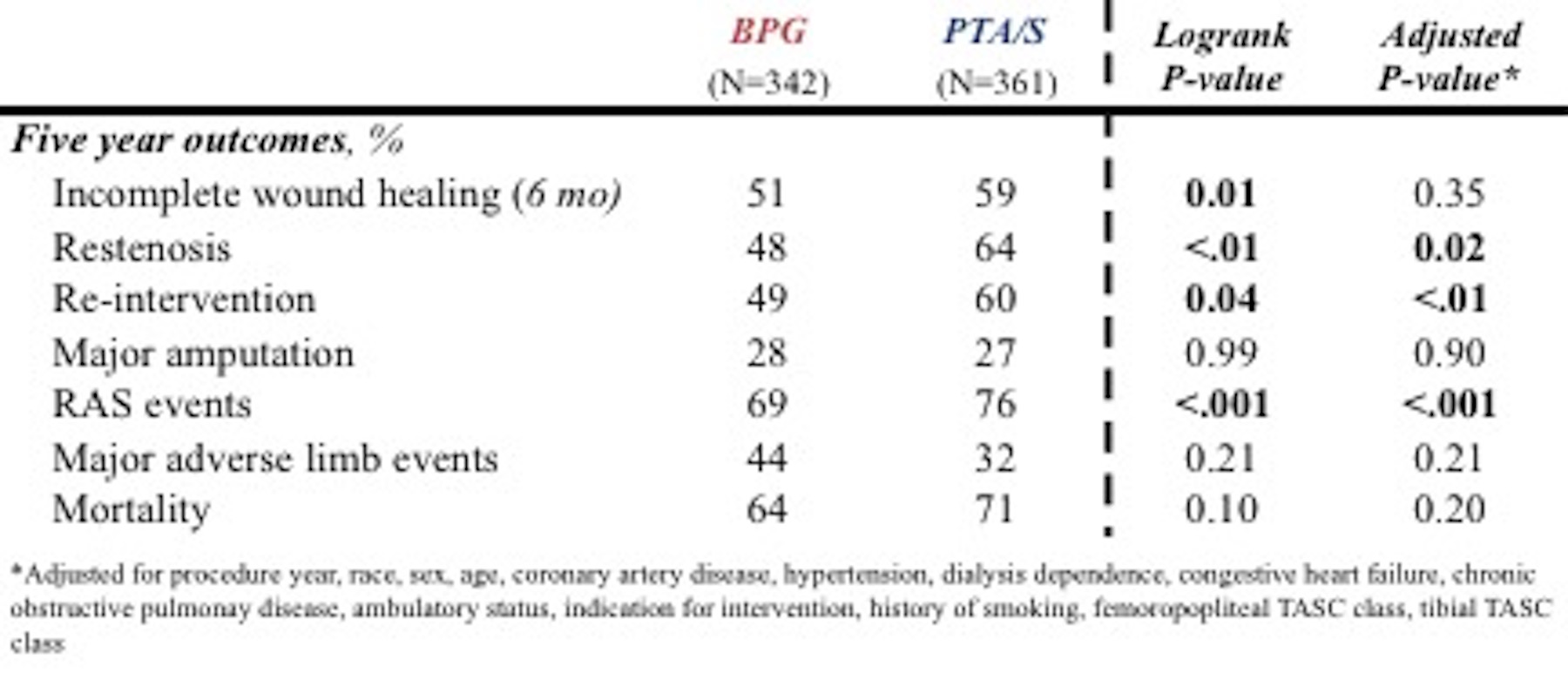
Back to 2018 Program




