Wound location is independently associated with adverse outcomes following first-time lower extremity revascularization for tissue loss
Jeremy D. Darling, M.S., Thomas F.X. O'Donnell, M.D., Sarah E. Deery, M.D., Giap H. Vu, B.A., Anthony V. Norman, B.S., Raul J. Guzman, M.D., Mark C. Wyers, M.D., Allen D. Hamdan, M.D., Marc L. Schermerhorn, M.D..
Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES: Few studies adequately evaluate the impact of wound location on patient outcomes following lower extremity revascularization. The aim of this study was to evaluate the relationship between lower extremity wound location and long-term outcomes in tissue loss patients undergoing any first-time lower extremity revascularization.
METHODS: We reviewed all patients at our institution undergoing either open surgical bypass or percutaneous transluminal angioplasty for tissue loss between 2005-2014. We categorized wounds into three distinct groups: forefoot (i.e., toes and metatarsal heads), midfoot (i.e., dorsal, plantar, lateral, medial surfaces not including toes, metatarsal heads, or heel), and heel. Limbs with more than one wound were excluded from analyses. We compared rates of perioperative complications, complete wound healing, limb salvage, amputation-free survival (AFS), and survival using Chi-square, Kaplan-Meier, and Cox regression analyses.
RESULTS: Of 2,869 infrainguinal revascularizations from 2005-2014, 630 limbs (forefoot=397, midfoot=61, heel=118) underwent a first-time revascularization for tissue loss with reliable information regarding wound specifics. Patients with forefoot, midfoot, and heel wounds were similar in age (71 vs. 69 vs. 70 years) and rates of coronary artery disease (54% vs. 60% vs. 48%), hypertension (86% vs. 85% vs. 86%), and smoking history (58% vs. 57% vs. 64%) (all P>.05). Conversely, there were significant differences seen in prevalence of gangrene (41% vs. 5% vs. 21%), diabetes (82% vs. 92% vs. 85%), and dialysis-dependence (18% vs. 17% vs. 30%) (all P<.05). Perioperative complications, including hematoma (5% vs. 10% vs. 8.5%), acute kidney injury (16% vs. 12% vs. 23%), and mortality (1.3% vs. 4.9% vs. 4.2%), did not differ (P>.05). Between forefoot, midfoot, and heel wounds, unadjusted 6-month rates of complete wound healing (69% vs. 64% vs. 53%) and 3-year rates of AFS (54% vs. 57% vs. 35%) and survival (61% vs. 72% vs. 41%) significantly differed (all P<.05) (Figure I). After adjustment, compared to forefoot wounds, heel wounds were associated with significantly lower rates of complete wound healing (HR 1.6; 95% Confidence Interval [1.1-2.2]), AFS (1.7 [1.1-2.8]), and survival (1.9 [1.1-3.2]).
CONCLUSIONS: Heel wounds confer considerably higher morbidity and mortality compared to midfoot or forefoot wounds in patients undergoing any first-time lower extremity revascularization. 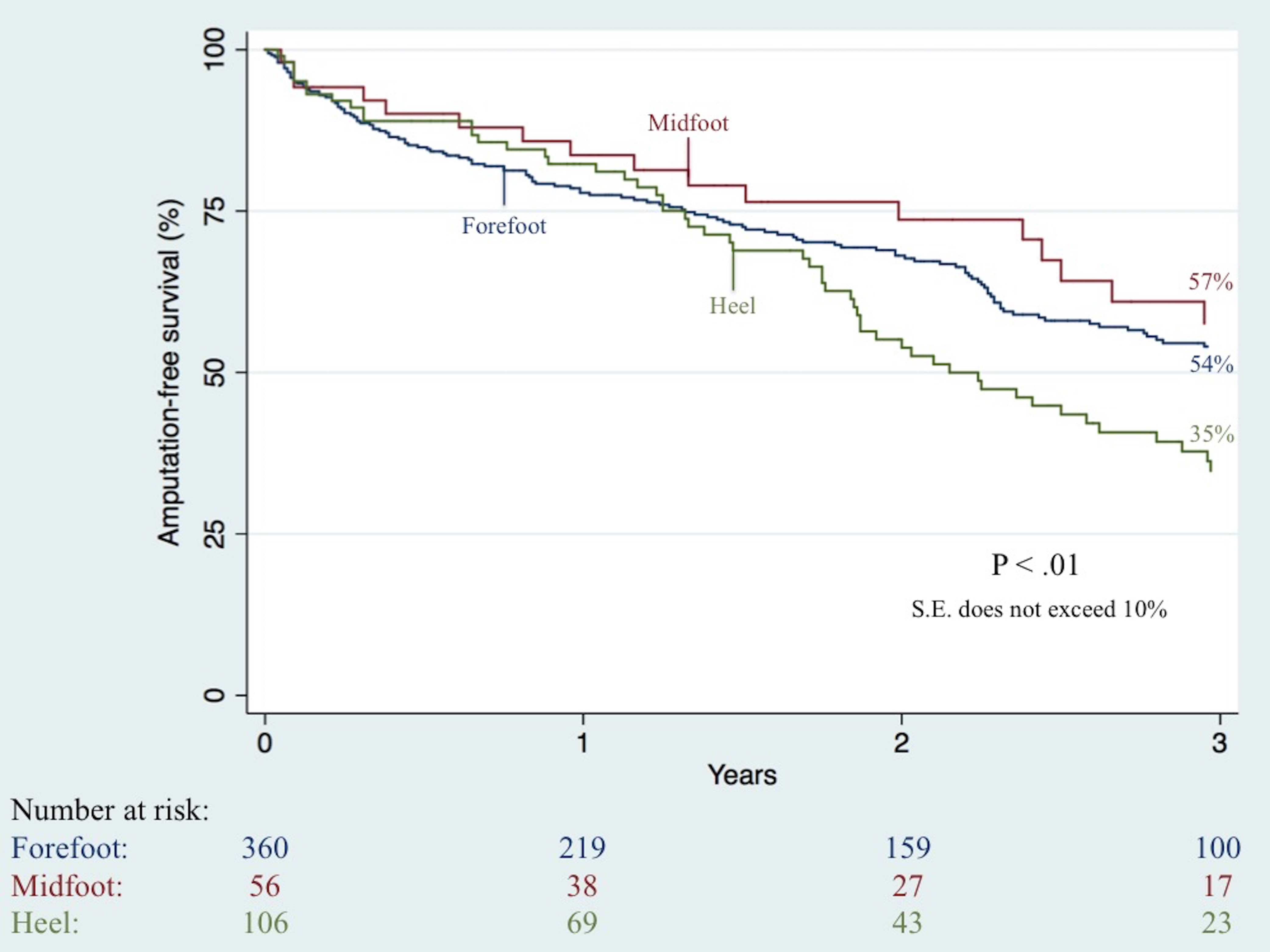
Back to 2018 Program




