Higher Mortality for Women with Peripheral Artery Disease
Samuel M. Miller1, Brandon J. Sumpio2, Alfredo C. Cordova, MD1, Bauer E. Sumpio, MD, PhD2.
1Warren Alpert Medical School of Brown University, Providence, RI, USA, 2Yale University Department of Vascular Surgery, New Haven, CT, USA.
Objective:
Gender differences in outcomes have been identified in patients with peripheral artery disease (PAD). We hypothesized that women with PAD would have equivalent morality with men following intervention.
Methods:
Patients with a primary diagnosis of critical limb ischemia (CLI) or claudication receiving open or endovascular intervention from 2003-2012 were identified from the Nationwide Inpatient Sample. Demographics, comorbidities, and mortality were analyzed by chi-squared tests of independence and independent-samples t-tests using SPSS 24 software. P<0.05 was considered statistically significant.
Results:
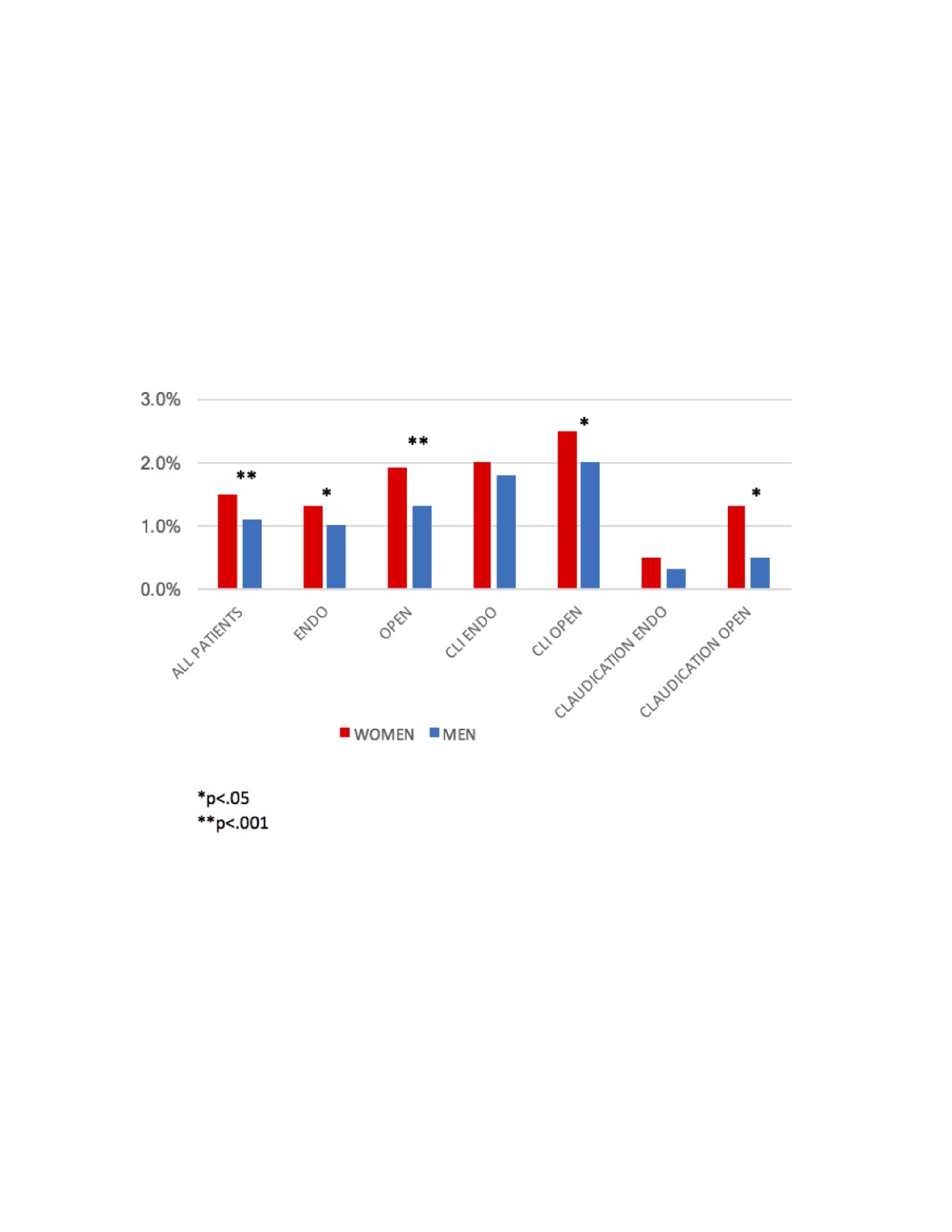
We identified 168,869 (71,171 women and 97,698 men) meeting the above criteria. Women were older than men (71.3 years vs. 68.0, p<.001). There were no differences in racial distribution but women had lower rates of diabetes (39.8% vs. 41.0%, p<.001), chronic obstructive pulmonary disease (18.0% vs. 19.4%, p<.001) and coronary artery disease (38.0% vs. 46.6%, p<.001), while having a higher rate of hypertension (59.5% vs. 55.7%, p<.001). There was no gender difference in the rate of chronic renal failure (3.2% vs. 3.4%, ns). Women had higher morality than men following surgical repair (1.5% vs. 1.1%, p<.001). When stratified by surgical technique, women also had higher mortality following endovascular repair (1.3% vs. 1.0%, p<.05) and open repair (1.9% vs 1.3%, p<.001). When separated by admitting diagnosis, women with CLI (2.5% vs. 2.0%, p<.05) and with claudication (1.3% vs. 0.5%, p<.05) had higher mortality than men following open intervention. There were no mortality differences seen in those with CLI (2.0% vs 1.8%, ns) or claudication (0.5% vs. 0.3%, ns) following endovascular surgery.
Conclusion:
Women had higher mortality than men after vascular intervention regardless of endovascular or open repair. However, subgroup analysis indicated that women with CLI or claudication demonstrated higher mortality following open compared to endovascular intervention. Treatment guidelines should include consideration of gender in their indications for surgical vascular repair, particularly for open repair.
Back to 2018 ePosters




