Endovascular Intervention Versus Open Bypass for the Treatment of Multilevel Critical Limb Ischemia: A Single Institution Propensity-Matched Study
John Futchko, MD, John Denesopolis, MD, Charles DeCarlo, MD, Patricia Friedmann, MS, Saadat Shariff, MD, Larry Scher, MD, Evan Lipsitz, MD, Karan Garg, MD.
Montefiore Medical Center, New York, NY, USA.
OBJECTIVES:
Endovascular therapies are increasingly applied in patients with complex multilevel disease and critical limb ischemia (CLI). Infrageniculate bypass is the mainstay of therapy in these patients. Data comparing matched patients for these groups is lacking. We compared outcomes between open and endovascular procedures for patients undergoing first time intervention for multilevel infrainguinal CLI at our medical center.
METHODS:
We retrospectively reviewed all patients undergoing first time endovascular or open surgical revascularization for multilevel CLI. Endovascular intervention included angioplasty, stenting, and/or atherectomy. Open intervention included autologous and nonautologous bypass. Interventions were performed at the surgeonís discretion. Primary endpoints were amputation-free survival (AFS), freedom from reintervention (FFR), and primary patency (PP). Propensity scoring was used to construct matched endovascular and bypass cohorts. Outcomes were evaluated using Kaplan-Meier and Cox Proportional Hazards models.
RESULTS:
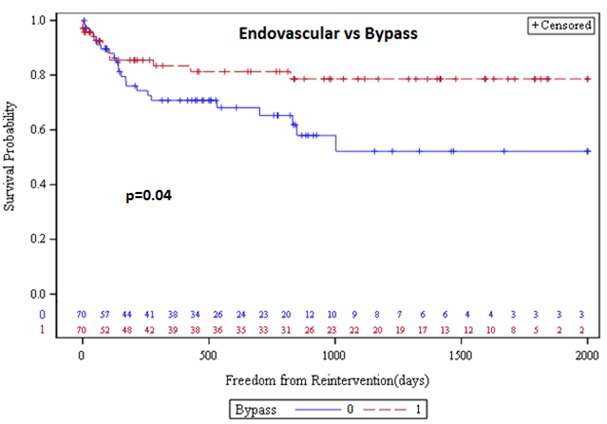
A total of 222 revascularizations in 217 patients were identified. There were 70 endovascular interventions and 152 bypasses (83 GSV, 69 PTFE). In matched analysis, there was no difference in perioperative death between the endovascular and open groups (1.4% vs 5.7%, p=0.37); however bypass patients had a higher incidence of perioperative myocardial infarction (0% vs 10.0%, p=0.01). Complete wound healing was achieved in a greater number of patients undergoing bypass than endovascular treatment (63.0% vs 37.0%, p=0.01). Kaplan-Meier analysis using propensity-matched bypass and endovascular cohorts revealed improved FFR for the bypass group (p=0.04, 81% vs 65% at 2 years), and no difference in AFS (p=0.96, 71% vs 65% at 2 years) or PP (p=0.44, 44% vs 52% at 2 years). In matched Cox analysis, endovascular intervention was not associated with improved limb salvage (HR 1.06, 95% CI 0.58-1.92). Major amputation was predicted by ESRD (HR 2.91, 95% CI 1.52-5.56). Propensity-matched comparison of endovascular intervention to nonautologous bypass demonstrated improved PP in the endovascular group (p=0.31).
CONCLUSIONS:
There was improved wound healing and fewer reinterventions in patients undergoing bypass surgery. Endovascular intervention as a first time revascularization for multilevel CLI offers no apparent benefit in AFS or PP compared to open revascularization. However, an endovascular approach may be preferred to open bypass when autologous conduit is unavailable.
Back to 2018 Program




