Comparison of Renal and Visceral Artery Aneurysms
Samuel M. Miller1, Brandon J. Sumpio2, Alfredo C. Cordova, MD1, Bauer E. Sumpio, MD, PhD3.
1Warren Alpert Medical School of Brown University, Providence, RI, USA, 2Yale University Department of Vascular Surgery, Providence, CT, USA, 3Yale University Department of Vascular Surgery, New Haven, CT, USA.
Objectives:
Renal artery aneurysms (RAA) and visceral artery aneurysms (VAA) are relatively rare entities and there are no large series comparing them. We hypothesized that patient characteristics, surgical interventions, outcomes and hospital charges are different between the two cohorts.
Methods:
Patients with a primary diagnosis of RAA or VAA, excluding those with concomitant aortic pathology, were identified from the Nationwide Inpatient Sample between 2003 and 2012. Demographics, comorbidities, repair techniques, complications and surgical outcomes were compared and analyzed by chi-squared tests of independence and independent-samples t-tests using SPSS 24 software. P<0.05 was considered statistically significant.
Results:
We identified 3402 patients, 2561 of whom had a primary diagnosis of VAA (splenic or non-splenic visceral artery aneurysms) and 841 with RAA. RAA patients were younger (57.1 years vs 58.7, p<.05) but there was no difference in gender distribution. RAA patients were more likely to have hypertension (52.3% vs 42.4%, p<.001) and chronic renal failure (2.0% vs 0.9%, p<.05), but less likely to have a dysrhythmia (9.8% vs 13.3%, p<.05) and peripheral vascular disease (0.4% vs 1.8%, p<.05). The rates of other comorbidities were not significantly different between groups (Table 1). A higher percentage of RAA patients were treated with endovascular repair but there was no difference in the number of patients managed conservatively in either group. RAA patients had lower mortality (2.1% vs 4.0%, p<.05) but experienced more postoperative acute renal failure (8.3% vs 5.4%, p<.05). Despite this, RAA patients had shorter lengths of stay in the hospital (5.2 days vs 7.1, p<.001) and lower hospital charges than those with VAA ($54,962 vs $74,961, p<.001).
Conclusion:
RAA patients have different demographics and comorbidities compared to VAA. Type of intervention and outcomes were also different between the cohorts. We conclude that based on these differences RAA and VAA patients should be considered as distinct clinical entities that cannot be grouped together because of their rarity. 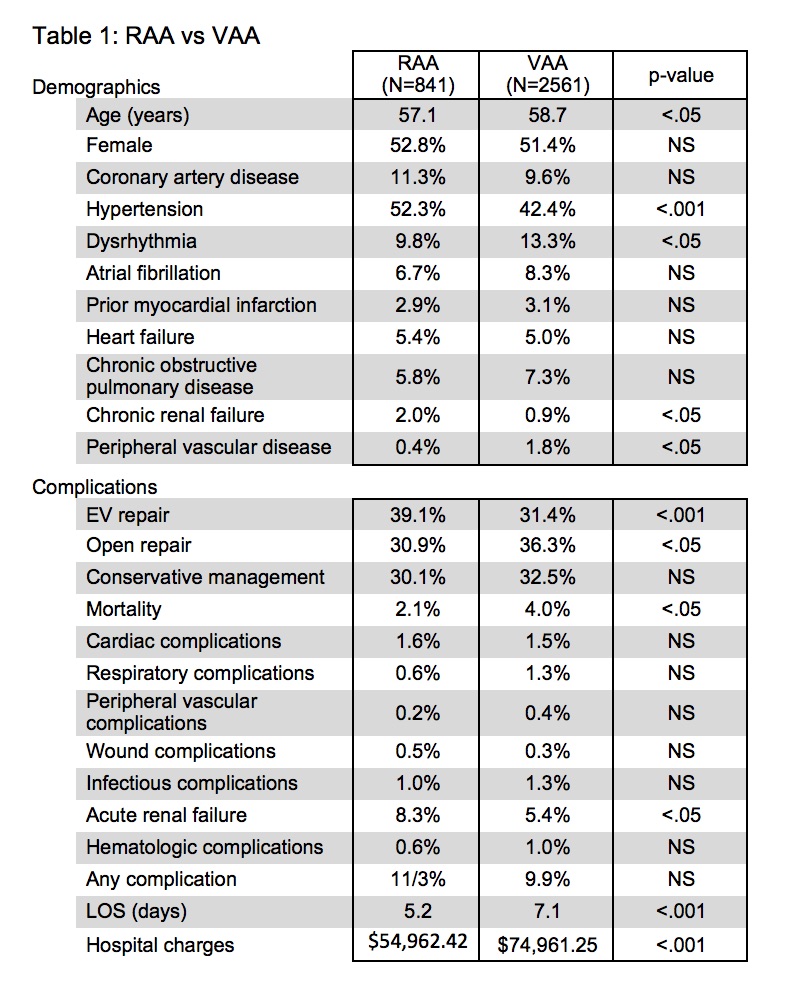
Back to 2018 Program




