Clinical and Financial Implications of Dementia in Vascular Surgery Patients
J Hunter Mehaffey, MD MSc, Robert B. Hawkins, MD MSc, Margaret Tracci, MD JD, William P. Robinson, MD, Ken Cherry, MD, John A. Kern, MD, Gilbert R. Upchurch, MD.
UVA, Charlottesville, VA, USA.
Introduction: Dementia represents a major risk factor for medical complications and has been linked to higher rates of complication after surgery. Given the systemic nature of vascular disease, medical comorbidities significantly increase cost and complications after vascular surgery. The purpose of this study was to assess the clinical and financial impact of dementia in patients undergoing vascular surgery.
Methods: The Vascular Quality Initative (VQI) database was queried for all patients undergoing vascular surgery at a single academic medical center 2012-2017. All modules were included (Open Abdominal Aortic Aneurysm, Suprainguinal Bypass, Lower Extremity Bypass, Amputation, Carotid Endarterectomy, Endovascular Aortic Aneurym Repair, Thoracic Endovascular Aortic Aneurysm Repair, and Peripheral Endovascular Intervention). An institutional clinical data repository was queried to identify patients with diagnosis codes for dementia as well as total hospital cost and long-term survival using the department of health social security records. Hierarchical logistic and linear regression models were fit to assess risk adjusted predictors of any complication and inflationadjusted cost. Kaplan Meier and Cox proportional hazards models were used for survival analysis.
Results: A total of 2308 patients underwent vascular surgey and were captured by the VQI over the past 5 years, with 88 (3.8%) having a diagnosis of dementia. Patients with dementia were older, had higher rates of medical comorbidities, and the most common procedure was major amputation. Additionally, dementia patients had significantly higher rate of any complication (52.3% vs 16.3%, p<0.0001) and increased 90-day mortality (13.6% vs 4.8%, p=0.0002). Furthermore, dementia significantly increased resource utilization including preoperative length of stay (LOS), postoperative LOS, intensive care unit LOS and inflation-adjusted total hospital cost (all p<0.0001). Hierarchical modeling demonstrated dementia was the strongest preoperative predictor for any complication (OR 8.64, p<0.0001) and had the largest risk-adjusted impact on total hospital cost (+$22,069, p<0.0001). Finally, survival analysis demonstrates dementia independently reduces survival after vascular surgery (HR 1.37, p=0.018, Figure).
Conclusions: This study demonstrates dementia is one of the strongest predictors of hospital cost and any complication after vascular surgery. Given the high risk of clinical and financial maladies, patients with dementia should be carefully considered and counseled prior to undergoing vascular surgery. 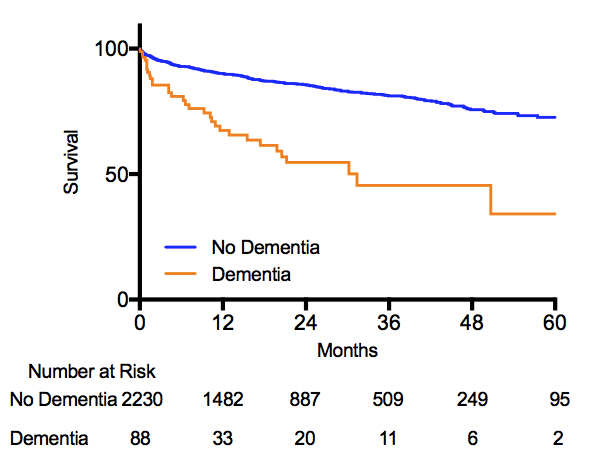
Back to 2018 Program




