High Volume Aortic Centers are Associated with Lower Mortality and Renal Complications in Open Juxtarenal AAA Repair
Laura T. Boitano, MD1, Thomas F.X. O'Donnell, MD1, Robert T. Lancaster, MD, MPH1, Jeffrey J. Siracuse, MD2, Marc L. Schermerhorn, MD3, Salvatore T. Scali, MD4, Richard P. Cambria, MD5, Virendra I. Patel, MD, MPH6.
1The Massachusetts General Hospital, Boston, MA, USA, 2Boston University School of Medicine, Boston, MA, USA, 3Beth Israel Deaconess Medical Center, Boston, MA, USA, 4University of Florida, Gainesville, Gainesville, FL, USA, 5St. Elizabeth’s Medical Center, Brighton, MA, USA, 6, New York Presbyterian / Columbia University Medical Center, New York, NY, USA.
OBJECTIVES: Previous studies identified a volume-outcome relationship in open infrarenal abdominal aortic aneurysm (AAA) repair. As juxtarenal AAA repair carries even higher morbidity and mortality than infrarenal repair, we studied the volume-outcome effect on intact, open juxtarenal AAA repair, and characterized differences in the use of protective intraoperative adjuncts between high and low volume centers.
METHODS: We identified all patients in the Vascular Quality Initiative (VQI) who underwent open repair of intact juxtarenal AAA between 2003-2017. We classified hospitals in the top two quintiles of average annual open aortic volume (both infrarenal and juxtarenal) as high volume (HVC, 26-95 cases/year), and the lowest three quintiles as low volume (LVC, 0-25 cases/year) centers. We used multivariable logistic and Cox regression to compare rates of perioperative events, use of intraoperative adjuncts, and mortality between high and low volume centers.
RESULTS: We identified 2,661 open intact juxtarenal AAA repairs from a total of 8,880 open AAA repairs, with 1,015 treated at HVC compared to 1,646 at LVC. HVC patients were more likely to be Caucasian, have congestive heart failure, and be on a statin. There was no difference in proximal clamp site; however, HVCs more often employed a retroperitoneal approach (47% vs. 35%; P<0.001), and anastomosed to the aorta distally (51% vs. 46%; P=0.01). After risk adjustment, treatment at a HVC was associated with more than twice the odds of receiving intraoperative renal cold perfusion (OR, 2.3 [95% confidence interval, 1.8-3.0]; P<0.001), and 30% higher odds of using mannitol (OR 1.3 [1.0 - 1.5]; P=0.03). Treatment at a HVC was associated with a 20% lower odds of any renal complication (OR 0.8 [0.6-0.9]; P=0.01) or being discharged to a facility (OR 0.8 [0.7-1.0]; P=0.03). In addition, patients at HVC had one-third the risk of 30-day death (OR 0.6 [0.5-0.8]; P=0.002), and significantly improved long-term survival (OR 0.7 [0.6-1.0]; P=0.02)(Figure).
CONCLUSIONS: Juxtarenal aneurysm repair at HVCs is associated with lower risk-adjusted operative mortality and renal complications. These results suggest societal benefit for regionalization of complex open aortic repair. 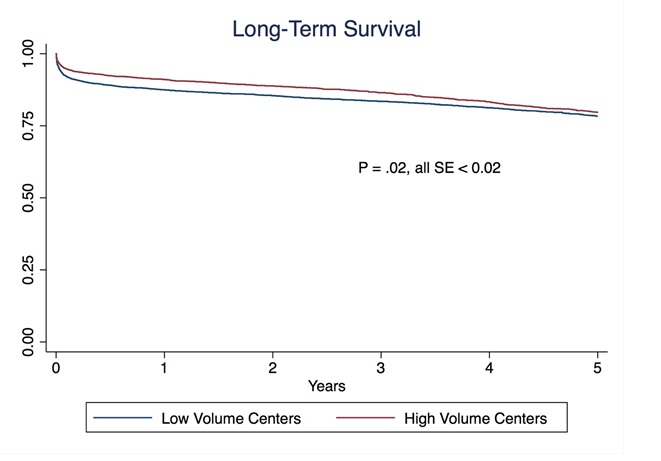
Back to 2018 Program




