Statin Therapy is Associated with Higher Long-term, but not Perioperative Survival after Abdominal Aortic Aneurysm Repair
Thomas FX O'Donnell, MD1, Sarah E. Deery, MD, MPH2, Katie E. Shean, MD1, Murray A. Mittleman, MD, Dr.PH3, Jeremy D. Darling1, Mohammad H. Eslami, MD4, Randall R. DeMartino, MD5, Marc L. Schermerhorn, MD1.
1Beth Israel Deaconess Medical Center, Boston, MA, USA, 2Massachusetts General Hospital, Boston, MA, USA, 3Harvard School of Public Health, Boston, MA, USA, 4University of Pittsburgh Medical Center, Pittsburgh, PA, USA, 5Mayo Clinic, Rochester, MN, USA.
Background: Although pre- and perioperative statin therapy improve postoperative outcomes in several populations, few data examine their association with survival following abdominal aortic aneurysm (AAA) repair. In addition, no data exist regarding the benefits of starting statins in patients with AAA not currently taking them.
Methods: We studied all patients undergoing repair of AAAs in the Vascular Quality Initiative between 2003 and 2017 without documented statin intolerance. We evaluated the association between preoperative statin therapy and long-term mortality, 30-day mortality, and in-hospital myocardial infarction and stroke. We also studied the cohort of patients not taking a statin preoperatively, and compared their long-term mortality based on whether or not they were discharged on a statin. To account for non-random treatment assignment, we constructed propensity scores and applied inverse probability weighting.
Results: We identified 40,452 AAA repairs, of which 37,950 fit our entry criteria (29,257 EVAR; 8,693 open). Overall, 25,997 patients (69%) took statins preoperatively. After propensity weighting, preoperative statin therapy was not associated with 30-day death; in-hospital stroke or MI. However, patients taking statins preoperatively experienced higher adjusted one-year (94% vs 90%) and five-year survival (85% vs 81%) from the date of surgery compared to those who were not (P<.001), although subgroup analysis showed this only applied to intact or symptomatic aneurysms. Of the 11,941 patients not taking a statin preoperatively and discharged alive, 2,910 (24%) started on a statin prior to discharge. In the subset of patients not on statins preoperatively, those initiated on a statin prior to discharge experienced higher survival at one year (94% vs 91%) and five years (89% vs 81%) (P<.001) than those who remained off statin therapy, with the greatest absolute long-term survival difference in patients with rupture (87% vs 62%, P<.001) (Figure 1).
Conclusions: Preoperative statin therapy is associated with higher long-term survival, but not perioperative mortality and morbidity, in patients undergoing AAA repair, and initiating statin therapy in previously statin-na´ve patients is associated with markedly improved survival. All patients with AAAs without contraindications should receive statin therapy. In patients not taking a statin at the time of AAA repair, clinicians should consider initiating one. 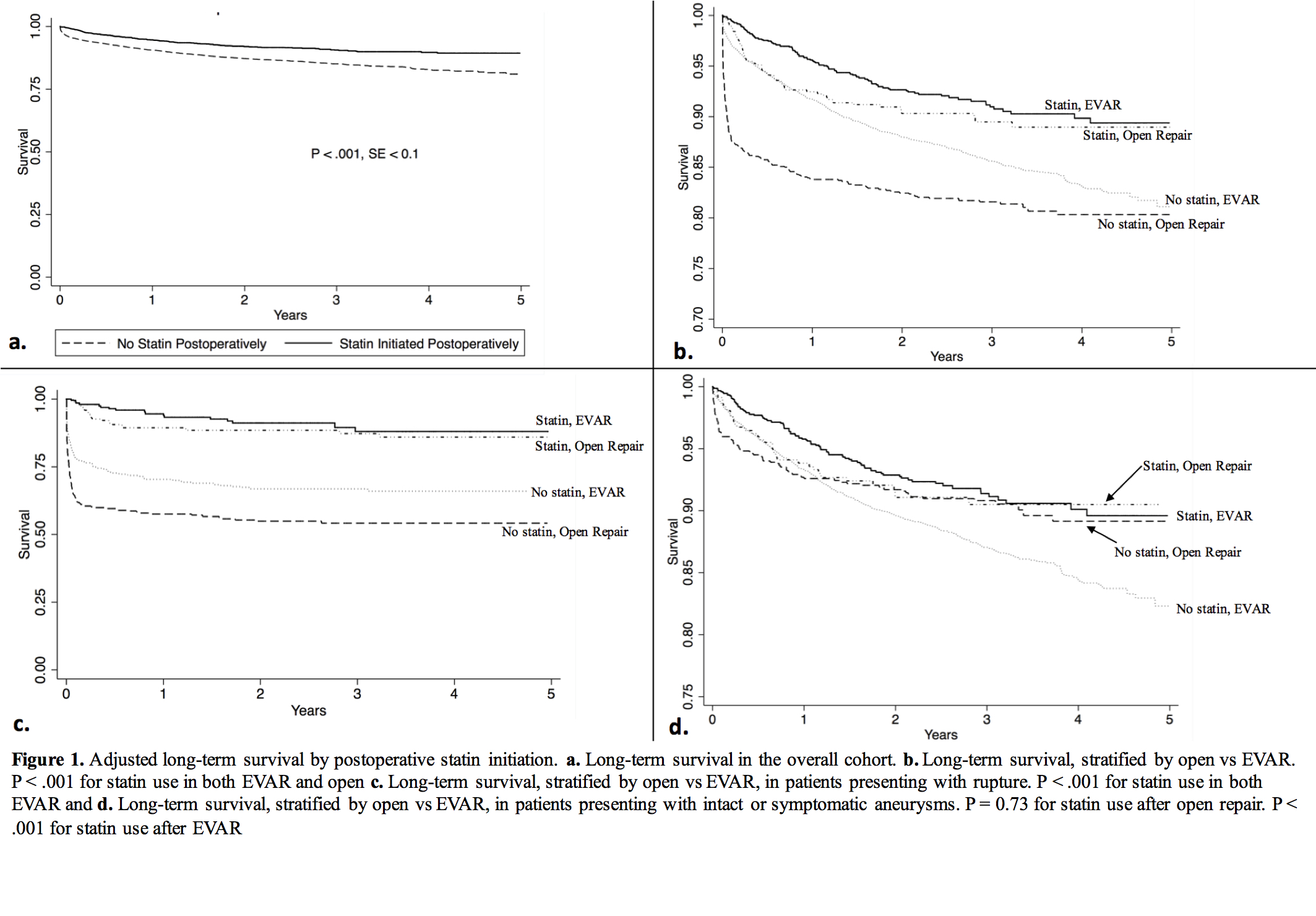
Back to 2018 Program




