Outcomes of open operative management of pararenal/paravisceral aortic infection
Indrani Sen, Manju Kalra, Gustavo Oderich, Thomas Bower, Peter Gloviczki.
Mayo clinic, Rochester, MN, USA.
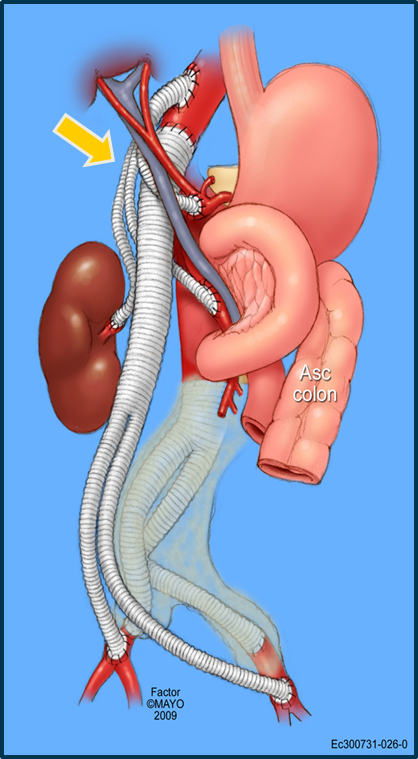
Introduction Operative management of pararenal/paravisceral aortic infection remains technically challenging. Our aim was to evaluate outcomes of operative management in these infections. Methods: Data from consecutive patients with infection involving the pararenal/paravisceral aorta undergoing open operative intervention between 1996- 2016 were retrospectively reviewed. Clinical features, imaging, operative details and morbidity were recorded. Primary end points were mortality, reinfection and patency. Results: Of 128 patients with aortic infection, 14 (12 male, 2 female, mean age 64 years) with pararenal or paravisceral infection were identified; 4 with distal thoracic aorta involvement. There were 5 primary mycotic aneurysms, 5 infected open aortic and 4 endovascular grafts. All patients were symptomatic; 2 presented with rupture. Surgical exposure was via midline laparotomy in 8 (58%); thoracoabdominal in 6. Aortic reconstruction was extraanatomic (Fig 1) in 8 [thoracic 6, intraabdominal 2;] and in situ in 6; conduits included Rifampin soaked polyester (11) and cryopreserved arterial graft (3). Operative adjuncts were partial left heart bypass and temporary axillary-femoral bypass (1 each). Concomitant renal and visceral bypasses were performed in 7 (n=24; 7 SMA, 5 celiac, 12 renal); renal bypasses (n=9) alone in 7 patients. Intra-operative cultures were polymicrobial (4), single organism (4) and sterile (5); 11/14 received antibiotics prior to presentation. In-hospital mortality was 4/14 (28%) due to multisystem failure. Morbidity included renal dysfunction requiring dialysis in 6 (including the 4 deaths); was transient in 2. Ischemic colitis occurred in 2 patietns, limb ischemia and myocardial infarction in 1 each. Average length of stay was 23 days (10-62 days). Following 6 weeks of intravenous antibiotics all patients received long term oral antibiotic suppression. Mean clinical and imaging follow-up were 33 (2-79) and 21 (8-68) months respectively. Three patients died during follow -up from unrelated causes. There were no graft complications or re-infection; at last follow up 2 grafts were not completely incorporated with no signs of infection. Conclusions: Operative management of aortic infection with involvement of the pararenal/paravisceral segment is complex. Though early mortality and morbidity are high in these sick patients, results in survivors are excellent with no long term sequelae and low risk of reinfection.
Back to 2018 Program




