Rates of Miscoding and Associated Costs with Elective Open versus Endovascular AAA Repair: A Single-Institution Retrospective Review
Suniah S. Ayub, MD, MPH1, Salvatore T. Scali, MD1, Julie A. Richter, MBA1, Thomas S. Huber, MD, PhD1, Javairiah Fatima, MD1, Adam W. Beck, MD2, Kristina A. Giles, MD1.
1University of Florida, Gainesville, FL, USA, 2University of Alabama, Birmingham, AL, USA.
OBJECTIVES:
EVAR costs are driven by implant charges and imaging surveillance. Open AAA repair(OAR) costs are driven by length of stay(LOS) and perioperative care. Few studies have explored miscoding to identify missed billing opportunities and impact on revenue.
METHODS: All elective infrarenal AAA repairs from 2010-15 were reviewed for MSDRG classification, comorbidities, complications, cost, and net collections. Average billing and reimbursement were standardized to Centers for Medicare and Medicaid Services(CMS) FY2014 data. MSDRGs were classified as "Standard" or "Complex" based on major complications/comorbidities(MCC). "MCC miscoding" were under-coding events where MCCs were present but not coded. "Non-specific miscoding" were assignments of MSDRG 253/254(‘Other Vascular Procedures’) instead of more specific MSDRGs(237/238/003). Total revenue(net collections-hospitalization cost) and lost billing opportunities were calculated based upon CMS data.
RESULTS: We reviewed 207 cases(EVAR-104;OAR-103). OAR patients had longer LOS, more perioperative complications, and higher mortality. OAR costs(median:$30,712) were similar to EVAR(median:$28,586;p=0.24). Implant costs differed significantly(EVAR-median:$13,183 vs. OAR,$623;p<0.0001). Despite similar comorbidities, more OARs were classified as complex(56% vs. EVAR, 14%;p<0.0001). Standard and complex patients had no differences in long-term survival(p=0.106). Complex patients had higher hospitalization costs, with median differences of $9,723(EVAR) and $16,725(OAR,p<0.0001). Of the 72 MCCs, 10 were comorbidities(EVAR-4;OAR-6) while 62 were complications(EVAR-10;OAR-52). Net collections between EVAR and OAR for standard and complex patients differed significantly. Revenue margins were negative for both standard/complex EVAR, but positive for OAR, with the greatest discrepancy between standard EVAR vs. OAR($4,163 difference,p=0.0005). Under-coding events included 14 "MCC miscoding"(EVAR-4;OAR-10) and 7 "non-specific miscoding"(EVAR-7;OAR-0). "Non-specific miscoding" led to greater median revenue loss(-$10,531) than "MCC miscoding"(-$3,261) or correct coding(-$276;p=0.003). Miscoding accounted for a total revenue loss of -$159,998. Net revenue for all patients was -$304,969. Using CMS data, miscoding represented a lost billing opportunity of $1,233,025. For all patients, potential lost CMS reimbursement was -$2,098,636, with no differences between miscoded vs. correctly coded patients(p=0.27).
CONCLUSIONS:
We demonstrated significant revenue discrepancy between EVAR and OAR, driven by differences in outcome, LOS, and patient complexity. With a 10% miscoding rate, we identified missed billing opportunities translating to lost revenue. Institutions must investigate causes of miscoding to improve operating margins and sustain AAA care delivery. 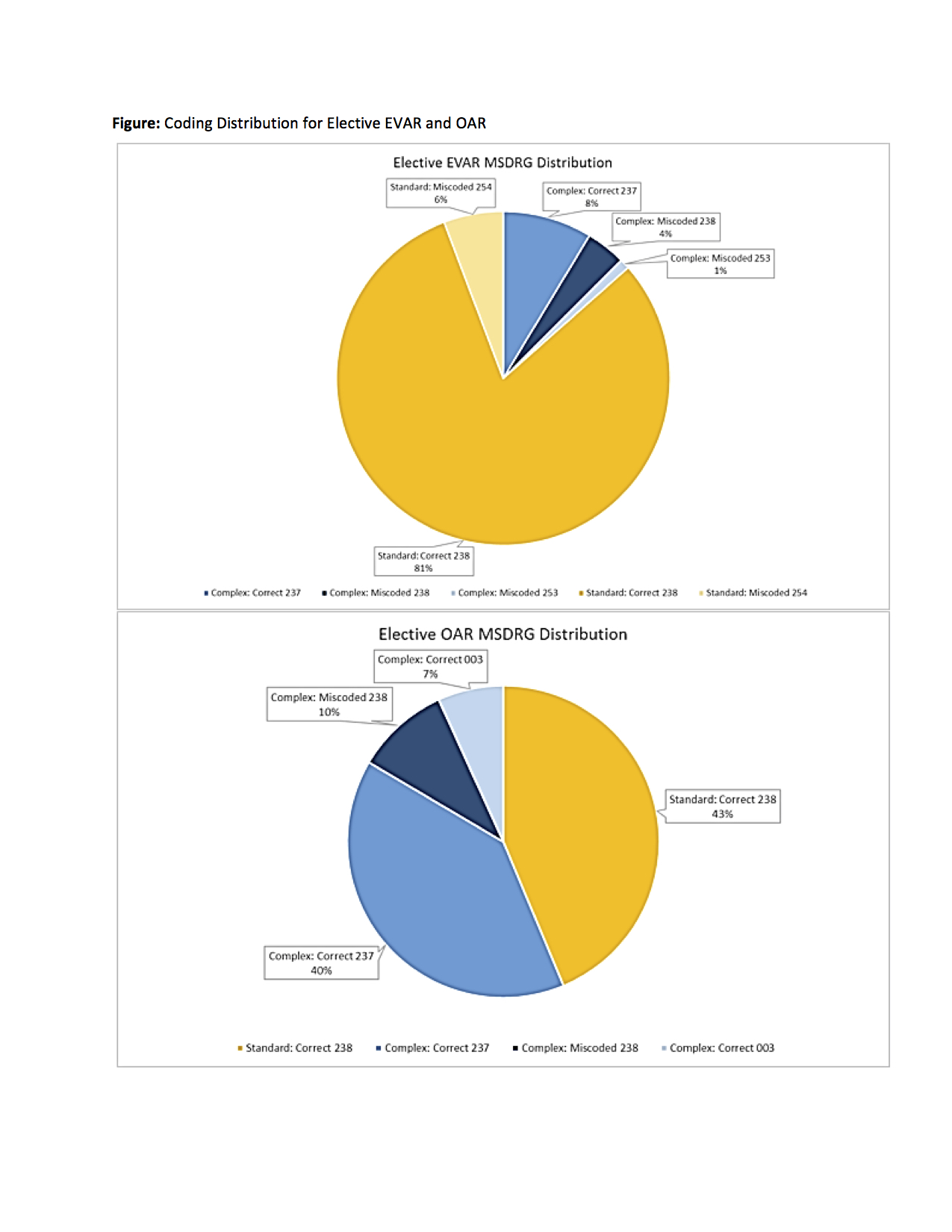
Back to 2018 Program




