Endovascular Repair of Thoracoabdominal Aneurysms Using a Novel Low Profile Multibranched Stent-Graft with Preloaded Guidewire Delivery System
Aleem K. Mirza, MD, Gustavo S. Oderich, MD, Giuliano Sandri, MD, Emanuel R. Tenorio, MD, PhD, Jan Hofer, RN, Jean Wigham, RN, Stephan Cha, MS, Blayne Roeder, PhD, Thanila A. Macedo, MD.
Mayo Clinic, Rochester, MN, USA.
Objectives: The aim of this study is to evaluate a novel low profile preloaded guidewire system (LP-PGS) multibranched stent-graft as compared to standard profile (SP) device without preloaded system.
Methods: We reviewed the clinical data of 386 consecutive patients enrolled in a prospective, nonrandomized investigational device exemption study to investigate F-BEVAR between 2007 and 2017 (NCT 1937949 and NCT2089607). Inclusion criteria was treatment for TAAAs with either SP multibranched stent-graft (t-Branch®, Cook Medical, Bloomington, IN) or patient-specific LP-PGS fenestrated-branched stent-graft. The PGS was accessible using a long delivery system, which exited via brachial access for sequential target vessel catheterization (Figure). End-points were technical success, operative data, mortality and major adverse events (MAEs).
Results: There were 42 patients (27 male, 73±9 years old) treated for TAAAs (37 Extent I-III and 5 Extent IV) using t-Branch® in 22 patients or LP-PGS stent-graft in 20 patients. A total of 160 renal-mesenteric vessels were incorporated (3.8±0.6 per patient). Patients treated t-Branch® stent-graft had larger aneurysms (80±9 vs. 65±10-mm, p=0.002), with 5 symptomatic or ruptured aneurysms. Technical success of target vessel incorporation was achieved in 100% (160/160), with no difference between t-Branch® and LP-PGS. Iliac conduits were needed in 4 patients (18%) treated by t-Branch® and in 3 patients (15%) with LP-PGS stent-graft (p=1). There was no difference in endovascular time (189±56 vs. 163±65 minutes; p=0.1), total operating time (278±65 vs. 250±78 minutes; p=0.22), fluoroscopy time (98±36 vs. 83±35 minutes; p=0.18), or contrast volume (199±77 vs. 158±57-mL; p=0.06) for treatment with t-Branch® or LP-PGS stent-grafts, respectively. Radiation exposure was lower for LP-PGS (3164±2497 vs. 1278±929 mGy; P=0.003). There were no deaths within 30-days or hospital stay. MAEs occurred in 9 patients (21%), with no difference between groups. At 1-year, patients treated by t-Branch® or LP-PGS stent-grafts had similar survival (81.5±8% vs. 88.9±10%, p=0.9), target vessel primary patency (100% vs. 95±5%, p=0.3), freedom from type I/III endoleak (89±7 vs. 100%, p=0.2), freedom from branch-instability (89.5±7 vs. 95±5%, p=0.7) and freedom from reintervention.
Conclusions: F-BEVAR using LP-PGS was performed with lower radiation exposure and was associated with a non-significant decrease in operating time, fluoroscopy and contrast use. 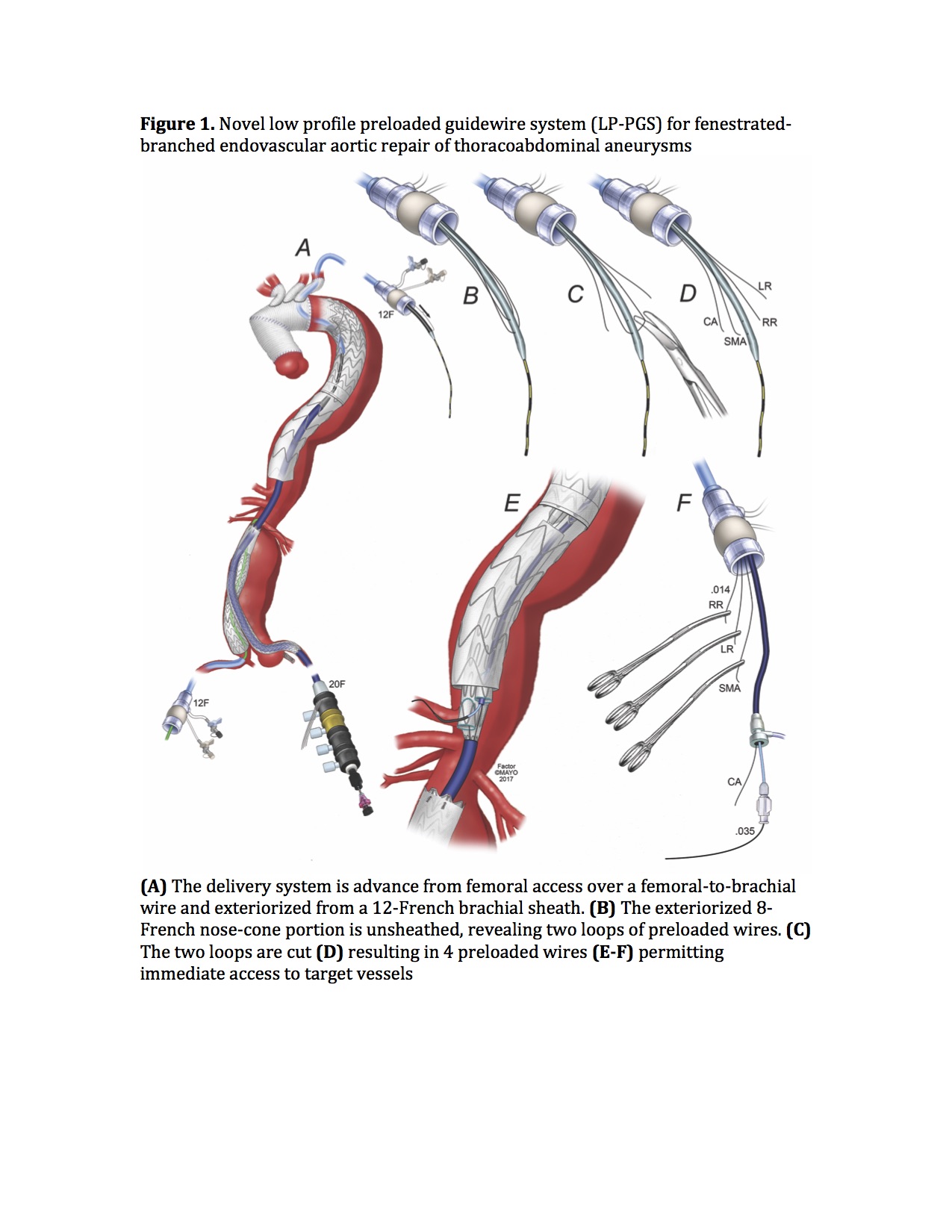
Back to 2018 Program




