TYPE II ENDOLEAKS MERIT ONGOING SURVEILLANCE DESPITE SUCCESSFUL INTERVENTION
Fahad Shuja, MB, BS1, Douglas W. Jones, MD2, Lars Stangenberg, MD, PhD2, Kirsten Dansey, MD2, Mark Wyers, MD2, Marc Schermerhorn, MD2.
1Mayo Clinic, Rochester, MN, USA, 2Beth Israel Deaconess Medical Center, Boston, MA, USA.
OBJECTIVES: To evaluate the outcomes of interventions for type II endoleaks after endovascular abdominal aortic aneurysm repair (EVAR).
METHODS: A retrospective analysis was performed of all interventions to treat isolated type II endoleaks between 2005 and 2015. Intervention for isolated type II endoleak was considered if there was a >5mm increase in maximum aortic diameter from post-procedure CT or from a subsequent smaller diameter if there was initial sac regression. Frequency of various techniques and re-intervention rate were calculated. Statistical analysis included comparing maximum aneurysm diameter before EVAR (Pre-EVAR), to size at the time of first intervention (Pre-intervention) and the last known diameter at the time of analysis (Post-intervention). Pre-Intervention to Post-intervention diameters were compared using paired t-test. Kaplan-Meier analysis was performed to estimate event rates over time.
RESULTS: A total of 126 interventions were performed in 59 patients with a mean follow-up of 33 months (range 7-110) after the first intervention. Mean interval between EVAR and first intervention was 21 months. Two patients presented with rupture related to persistent type II endoleak. Survival was 92% at 3 years. There were no aneurysm-related deaths. Re-intervention was performed in 46% patients with a mean of 2.1±1.3. procedures per patient. The 3 year cumulative freedom from re-intervention was 62±5.7%. Types of intervention included transfemoral lumbar embolization (65%), transcaval embolization (25%), IMA coiling (19%), trans-lumbar sac embolization (9%),and open (sacotomy and lumbar/IMA ligation with graft preservation [2%] or graft explantation [2%]). Peri-procedural complications were seen in 5% of patients. There was a statistically significant difference between Pre-EVAR and Pre-intervention aortic diameters (Figure). Post-Intervention diameters were decreased compared to Pre-intervention, but remained higher than Pre-EVAR values. At 3 years, 10% had sac regression, 56% were stable, and 34% had sac expansion.
CONCLUSIONS: Treatment of type II endoleak remains a significant challenge with a high rate of re-intervention. These interventions are associated with sac regression, however, the mean aneurysm diameter remains enlarged compared to Pre-EVAR values. Long-term surveillance and selected intervention are recommended due to the risk of aortic rupture from persistent type II endoleak. 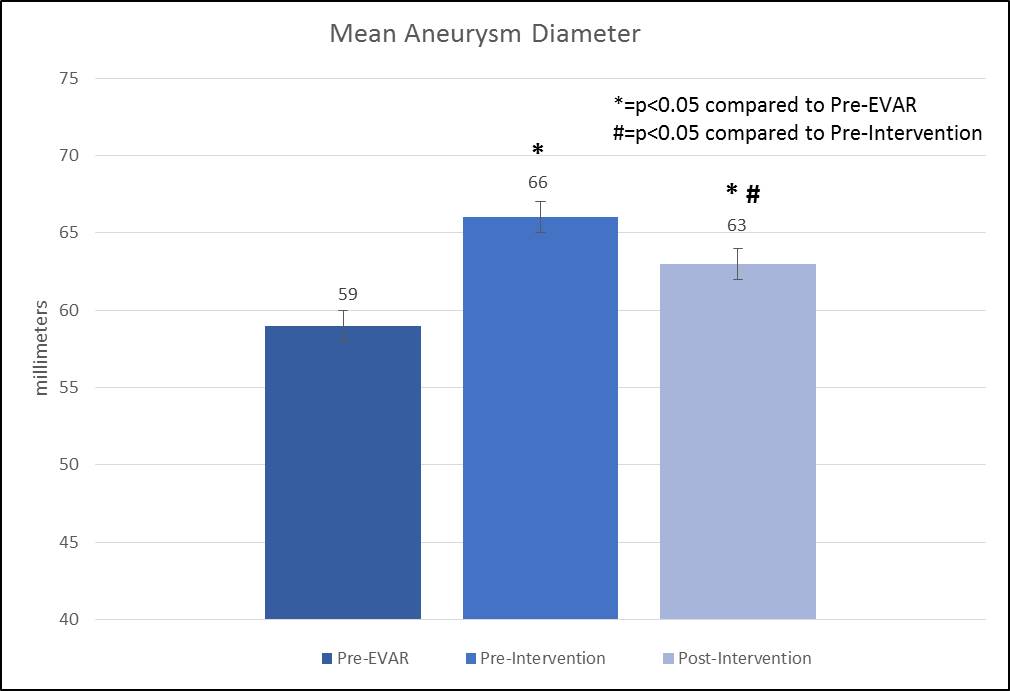
Back to 2018 Program




