Predicting Postoperative Destination through Preoperative Evaluation in Elective Open Infrarenal Abdominal Aortic Aneurysm Repair
Laura T. Boitano, MD, James C. Iannuzzi, MD, MPH, Jahan Mohebali, MD, MPH, Adam Tanious, MD, MMSc, Samuel I. Schwartz, MD, W. Darrin Clouse, MD, Mark F. Conrad, MD, MMSc.
The Massachusetts General Hospital, Boston, MA, USA.
OBJECTIVES: There are limited data guiding preoperative counselling on the need for discharge to skilled nursing facilities (NHD) following elective open infrarenal abdominal aortic aneurysm repair (OAR). This study aims to determine the preoperative predictors for NHD.
METHODS: The National Surgical Quality Improvement Program Vascular Procedure Targeted database was queried for elective OAR from 2011-2015. The primary endpoint was discharge to home or NHD. Complex surgery was defined as high operative time (top quintile of operative time), or procedure including lower extremity revascularization (LER). A multivariable logistic regression model was used to identify preoperative factors predictive of NHD.
RESULTS: Overall 581 patients were included; 101 (17%) required NHD. Baseline characteristics differed as follows: patients discharged to NHD were more frequently female, older (74.8±7.9 vs. 68.3±8.9 years; P<0.001), had history of COPD, a bleeding disorder or anemia. Patients requiring NHD were also more likely to have partial or full dependence at baseline. Complex surgery was associated with NHD indicated by greater proportion of high operative time cases (30% vs. 20%;P=0.03), and greater proportion needing LER (17% vs. 8%;P=0.003). After risk adjustment, females were 2x more likely to require NHD (OR:1.8,[95% confidence interval(CI), 1.1-3.0];P=0.02), age>80 years had 13x the odds for NHD (OR:13.1,CI:3.6-47.5; P<0.001), and septuagenarians had 9x the odds (OR;9.0,CI2.7-30.7;P<0.001). Partial dependence was associated with an 8 fold increase in discharge to NHD (OR:8.5,CI:1.46-49.1;P=0.02). History of a bleeding disorder trended towards a significant predictor of NHD (OR:2.1,CI:0.97-0.48;P=0.06). More complex repair remained a significant predictor of NHD after risk adjustment including LER (OR:2.7,CI1.4-49.1;P=0.004) and high operative time (OR:1.8,CI:1.0-3.0;P=0.05)(table 1).
CONCLUSIONS: Discharge to NHD following OAR can be predicted using preoperative factors. Preoperative identification of patients at high risk for NHD can help define expectations, and facilitate early referral to skilled facilities.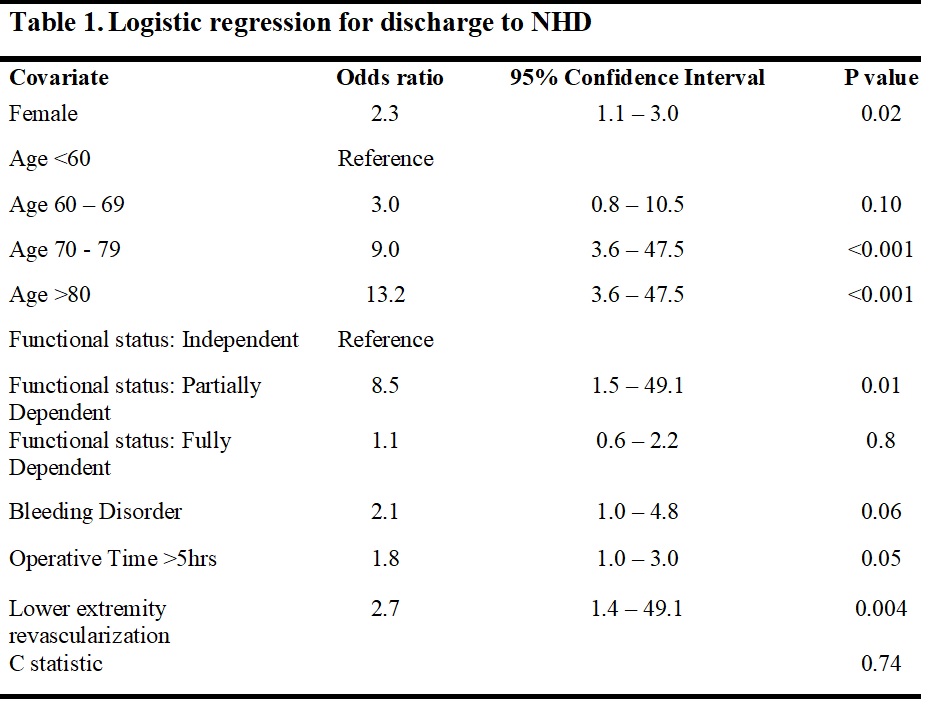
Back to 2018 ePosters




