Who Should Fix the Bowel?
Adam Tanious, MD, MMSc, Christine Jokisch, MD, Hillary McMullin, BS, Mathew Wooster, MD, Paul A. Armstrong, DO, Murray L. Shames, MD.
University of South Florida, Tampa, FL, USA.
Introduction:
Infected aortic grafts involving the bowel call for concomitant vascular and general surgical skills. We sought to understand patient outcomes based on who performed the bowel repair and as well as the effects of bowel complications in this patient cohort.
Methods:
Patients were selected using CPT codes for repair of graft-enteric fistulas as well as excision of infected abdominal grafts requiring concomitant bowel surgery between 2002-2015. Surgeons were broken up into vascular surgeons or bowel surgeons (including general, trauma, and colorectal surgeons). Bowel injuries were defined as simple or complex (depending on whether resection and anastomosis were required) as well as by the number of injured segments (single versus multi-segment). Hospitalization and follow-up data were analyzed with univariate and multivariate regression models.
Results:
Table 1 displays overall cohort demographics/characteristics for the 44 patients treated. Vascular surgeons performed their own bowel repair in 62% of index cases for this cohort (n = 26). Looking specifically at the repairs performed, bowel surgeons were required to operate on multiple segments of the bowel in 50% of cases while vascular surgeons had single bowel-segment injuries in 80% of cases (P = .0489). More than half of the bowel repairs by vascular surgeons were primary bowel repairs (56%), whereas bowel surgeons performed complex repairs requiring resections and anastomosis in 67% of their patient cohort.
Vascular surgeons did have an overall higher bowel complication rate as compared to non-vascular surgeons (30% vs 18%) though it was not significantly different (p = 0.7). Multifactorial logistic regression showed that mortality was significantly affected by having a post-operative bowel complication (P = .0247). The mortality odds ratio for those with a post-operative bowel complication was 7.6 as compared to those without a bowel complication (P = .0342).
Conclusion:
Aorto-enteric fistulas remain a devastating pathology. Traditionally trained vascular surgeons have higher bowel complication rates as compared to bowel surgeons. Post-operative bowel complications significantly affect the overall mortality of this patient population. 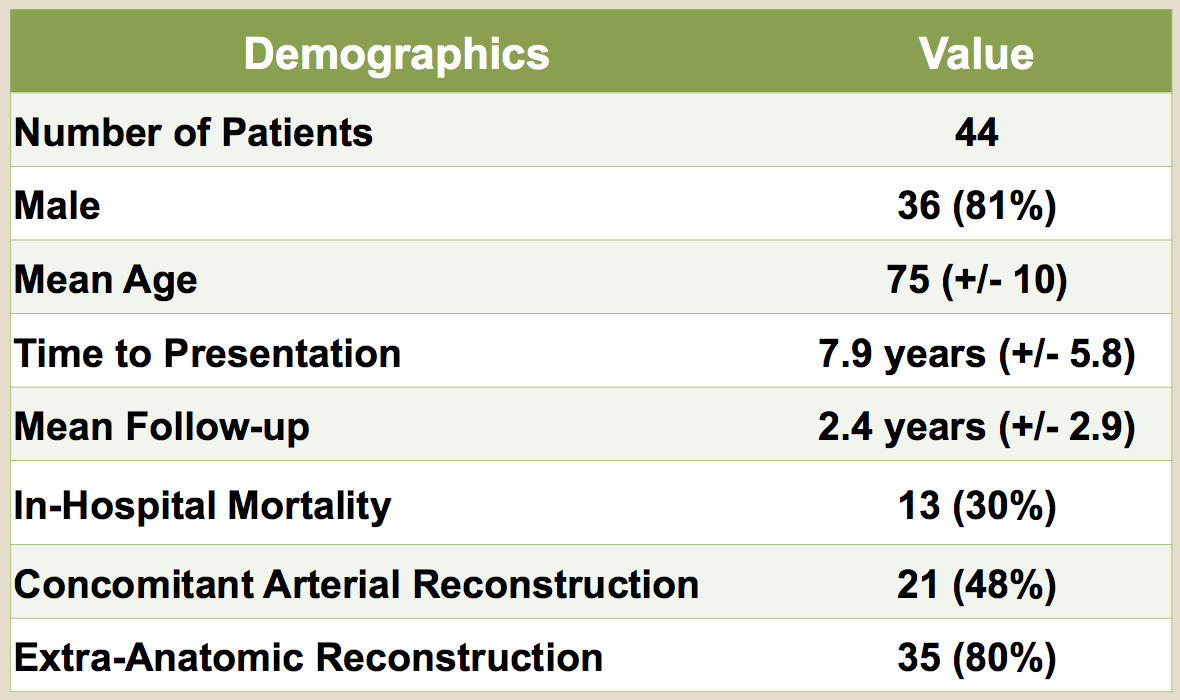
Back to 2018 ePosters




