Risk Calculator Tool for In-hospital Adverse Events following Endovascular Aortic Aneurysm Repair
Besma J. Nejim, MBChB MPH1, Devin Zarkowsky, MD2, Caitlin W. Hicks, MD MS1, Muhammad Faateh, MD1, James H. Black, III, MD1, Mahmoud B. Malas, MD MHS1.
1Johns Hopkins University School of Medicine, Baltimore, MD, USA, 2University of Southern California San Francisco, San Francisco, CA, USA.
Objectives: The aim of this study was to identify the predictors of in-hospital events following elective endovascular repair of abdominal aortic aneurysms. EVAR-related mortality has been exhaustively studied but little is known about the determinants of in-hospital morbidities following EVAR.
Methods: The Vascular Quality Initiative EVAR database (2003-2016) was explored. Patients who had non-elective repair, intraoperative death or were converted to open repair were excluded. In-hospital events (IHE) were defined as any in-hospital myocardial infarction, stroke, pneumonia, respiratory failure, renal failure, lower extremity ischemia, bowel ischemia, or reoperation. Backward selection based on the AIC statistic was implemented to select the predictors of IHE from the multivariable logistic regression (MLR) model. Receiver Operating Curves (ROC) were used to assess the final model. A graphical risk probability calculator (nomogram) was constructed as a post-estimation of the MLR model.
Results: 24,550 patients undergoing EVAR were included, of which an IHE occurred in 1,628 (6.6%). Patients with IHE were slightly older [mean age (±SD): 75.6(±8.2) vs 73.4 (±8.5); P<.001] and more frequently female (26.7%vs.18.0%; P<.001). Comorbid conditions were more prevalent in patients who developed IHE such as diabetes, hypertension, CKD, COPD, and CHF (All P<.05). The selected predictors of in-hospital events were GFR<60 [strongest predictor; adjusted odds ratio(95%CI): 1.89(1.69-2.11); P<.001], CHF [aOR(95%CI): 1.88(1.38-2.56); P<.001], COPD, blood transfusion, contrast volume, female gender, increasing age, diabetes, increasing aneurysm diameter by one centimeter [aOR(95%CI): 1.15(1.10-1.22); P<.001], and HTN (weakest predictor). Area under the curve was 72.5%. A nomogram was constructed from the MLR demonstrating a score for each predictor of IHE. A summation of the predictor scores is the total
patient score (range: 1.7-30.2); a patient with a score of 3 will have a 1% probability of IHE, whereas a patient with a score of 9 will have a 30% probability of IHE (Figure).
Conclusion: This study provides insights about the potential risk factors for postoperative complications following EVAR. We have introduced a risk calculator tool to assist surgeons in determining individual patients’ risk of developing IHE. The risks and benefits of intervention should be discussed and weighed beforehand for patients at higher risk for IHE post-EVAR 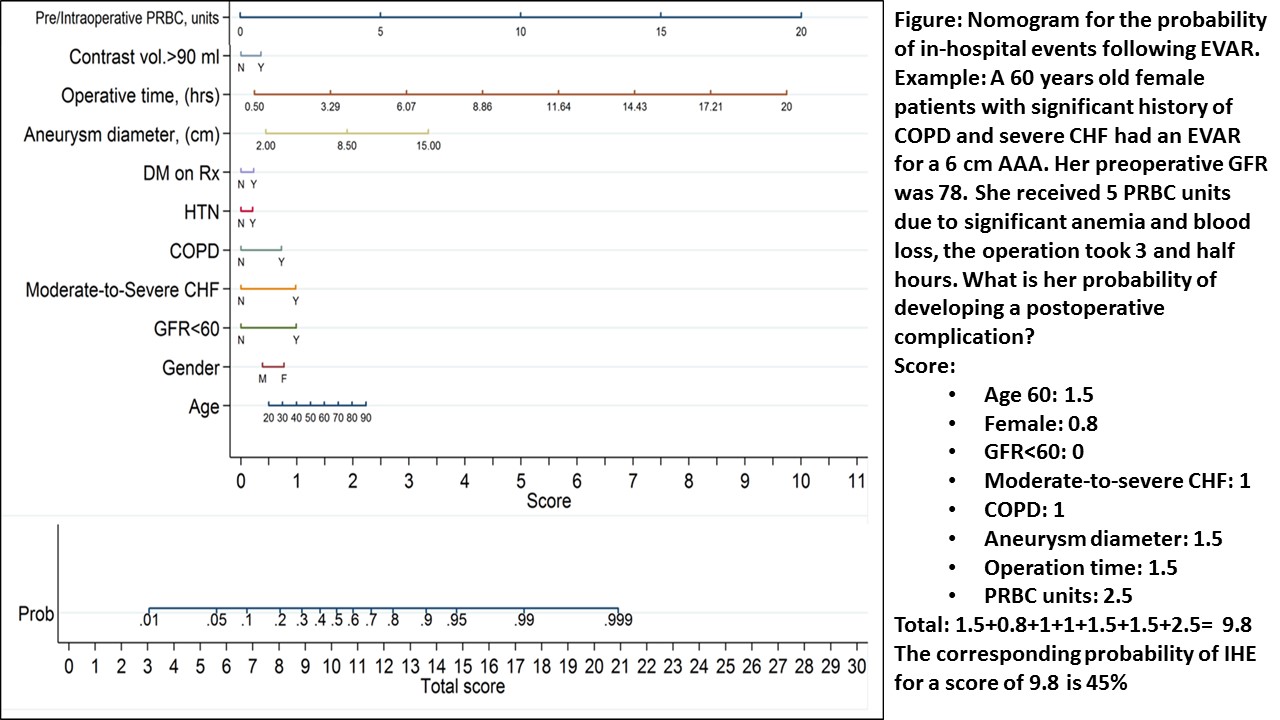
Back to 2018 ePosters




