The Effect of Clinical Coronary Disease Severity on Outcomes of Carotid Endarterectomy with and without Combined Coronary Bypass
Linda J. Wang, MD, MBA1, Jahan Mohebali, MD, MPH1, Philip Goodney, MD, MS2, Virendra Patel, MD, MPH3, Mark Conrad, MD, MMSc1, Matthew Eagleton, MD1, W. Darrin Clouse, MD1.
1Massachusetts General Hospital, Boston, MA, USA, 2Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA, 3Columbia University, New York, NY, USA.
Objectives: The management of patients with carotid stenosis and symptomatic coronary disease (CAD) is challenging. This study assesses the impact of clinical coronary disease severity on carotid endarterectomy (CEA) with and without combined coronary bypass (CCAB).
Methods: Using the Vascular Quality Initiative, patients with symptomatic CAD who underwent CCAB or isolated CEA (ICEA) from 2003-2017 were identified. Patients were stratified by CAD severity: stable angina (SA) and recent MI/unstable angina (UA). Primary outcomes, including perioperative stroke, MI, and stroke/death/MI (SDM), were assessed between procedures within each CAD cohort.
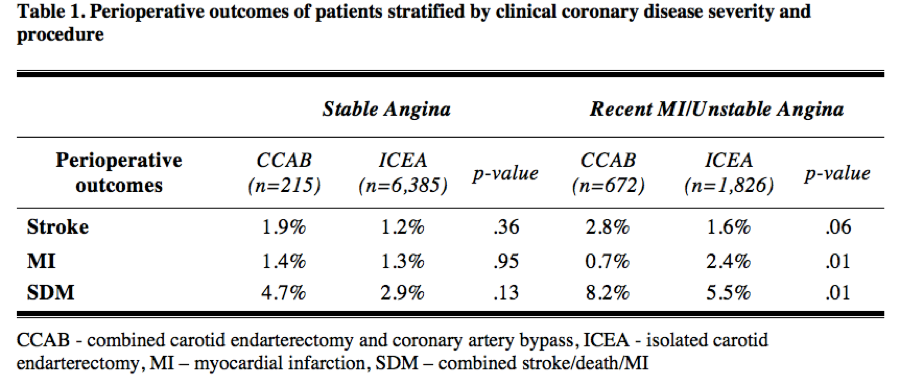
Results: 9,098 patients were identified: 887 CCAB [215 (24%) SA, 672 (76%) UA] and 8,211 ICEA [6,385 (78%) SA, 1,826 (22%) UA]. Overall, CCAB had higher rates of stroke (2.6% vs 1.3%, p=.002) and SDM (7.3% vs 3.5%, p<.001), but similar rates of MI (0.9% vs 1.6%, p=.12) compared to ICEA. In SA, no difference was seen in stroke (ICEA 1.2% vs CCAB 1.9%, p=.36), MI (1.3% vs 1.4%, p=.95), or SDM (2.9% vs 4.7%, p=.13). In UA, no difference was seen in stroke (ICEA 1.6% vs CCAB 2.8%, p=.06), but ICEA had higher rates of MI (2.4% vs 0.7%, p=.01) and CCAB had higher rates of SDM (5.5% vs 8.2%, p=.01). (Table 1) After logistic regression in the UA cohort, predictors of MI included ICEA (OR 2.8, 95%CI 1.1-7.1, p=.03) and symptomatic status (OR 2.0, 95% CI 1.1-3.6, p=.02); symptomatic status also predicted stroke (OR 1.9, 95%CI 1.04-3.6, p=.04), but CCAB did not.
Conclusions: In patients with symptomatic CAD, both clinical CAD severity and operative strategy affect outcomes. In SA patients, CCAB does not increase perioperative morbidity. However, CCAB in UA patients prevents MI while not appreciably increasing stroke risk. This suggests coronary revascularization prior to or concomitant with CEA should be considered in UA patients, but that temporally prioritizing the treatment of one vascular bed over the other is less important in SA patients.
Back to 2019 Abstracts
