Outcomes of directional branches using self-expandable versus balloon-expandable stent-grafts during endovascular repair of thoracoabdominal aortic aneurysms
Emanuel R. Tenorio, MD, PhD, Jussi M. Kärkkäinen, MD, PhD, Bernardo C. Mendes, MD, Randall R. DeMartino, MD, Jean Wigham, RN, Alisa Diderrich, RN, Jan Hofer, RN, Gustavo S. Oderich, MD.
Mayo Clinic, Rochester, MN, USA.
Purpose: To evaluate outcomes of directional branches using self-expandable (SESG) or balloon-expandable (BESG) stent-grafts during fenestrated-branched endovascular aortic repair (F-BEVAR) of thoracoabdominal aortic aneurysms (TAAAs).
Methods: Patients treated with F-BEVAR in a prospective study using directional branches were included in the study. Choice of bridging stent evolved from SESG to BESG (Gore VBX®, Flagstaff Arizona) in February 2017. Target artery instability (TAI) was defined by stent occlusion, stenosis, separation, type IC/IIIC endoleak, reintervention, rupture or death due to target artery complication. End-points included technical success, target artery patency and freedom from TAI, type IC/IIIC endoleak and reintervention.
Results: There were 118 patients (60% male, mean age 75±7 years) with 296 renal-mesenteric arteries targeted by directional branches using SESGs in 69 patients/162 arteries or BESGs in 49 patients/134 arteries. Patients with both groups had similar aneurysm diameter, target artery diameter and TAAA extent, which was I-III in 90%. Patients treated by SESGs had significantly (P<.05) shorter stent length (-7mm), larger stent diameter (+1mm) and more adjunctive bare metal stents (BMSs, 74% vs 10%). Technical success was achieved in all patients with no 30-day mortality. Mean follow up was significantly longer among patients treated by SESGs (19±12 vs 6±5 months). TAI occurred in 19 directional branches (6%), including two stent occlusions (all SESGs), five stenosis (3 SESGs, 2 BESG), two separations (all SESGs), nine type IC endoleaks (2 SESGs, 7 BESGs) and four type IIIC endoleaks (3 SESGs, 1 BESG), resulting in 15 reinterventions. At 1-year, there was no difference in primary (97±1% vs. 98±1%, P=.77) and secondary patency (99±1% vs. 100%, P=.38) for SESGs and BESGs, respectively. However, SESGs had higher freedom from TAI (96±2% vs. 90±4%, P=.005), type IC/IIIC endoleaks (98±1% vs. 91±3%, P=.003) and reinterventions (96±1% vs. 92±4%, P=.02) compared to BESGs (Table). Factors associated with TAI were renal artery target (OR 2.8, P=.03) and lack of adjunctive BMS (OR 0.2, P=.004).
Conclusion: Directional branches were associated with high technical success and low rates of occlusion or stenosis, independent of stent type. However, freedom from TAI was lower for BESGs due to more target artery endoleaks. 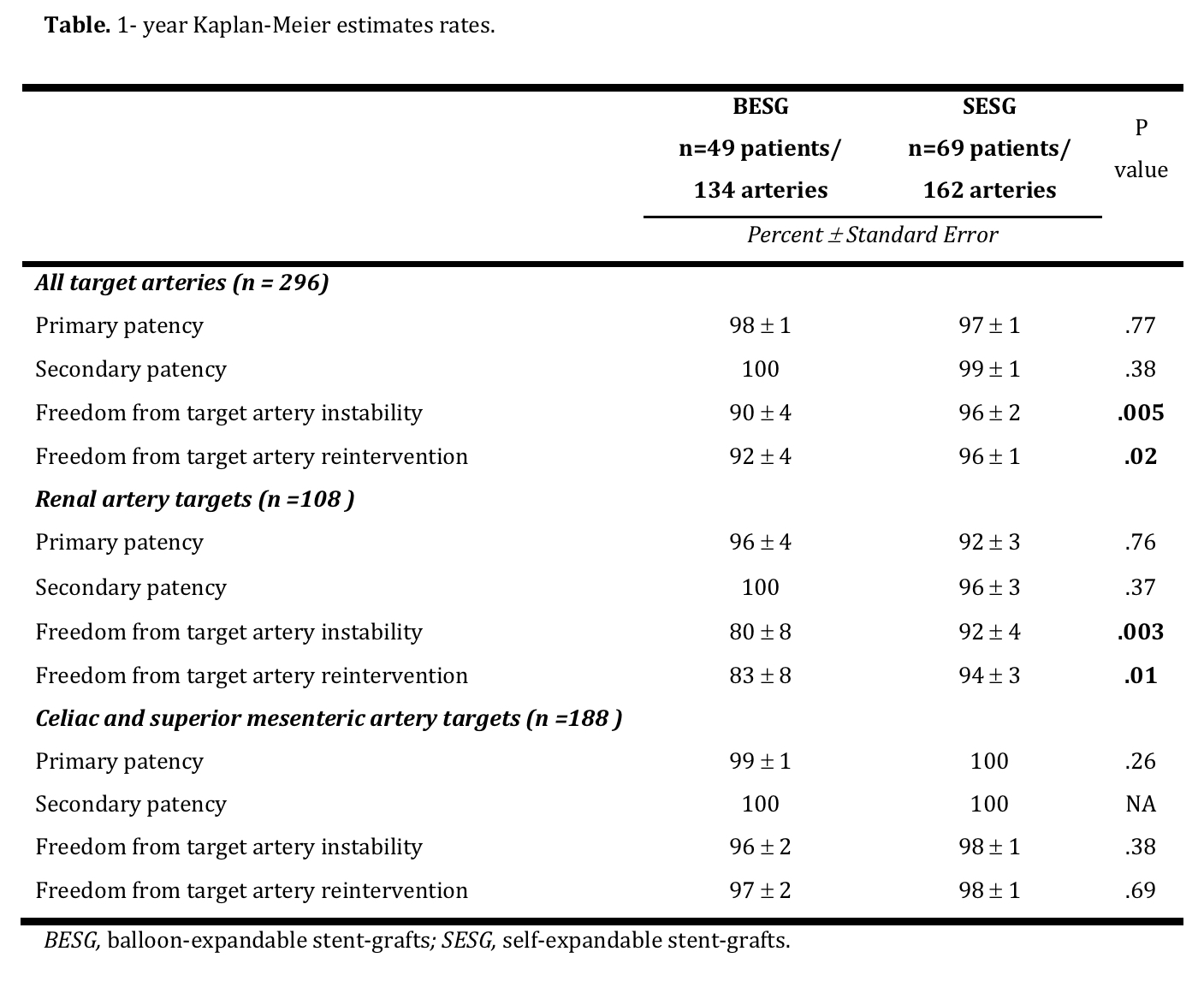
Back to 2019 Abstracts
