Poor Medical Management, Atherectomy and Multilevel Therapy are Associated with worse Outcomes after Endovascular Interventions for Claudication
Jonathan Bath1, Peter F. Lawrence2, Dan Neal3, Yuanyuan Zhao3, Adam W. Beck4, Michael Conte5, Marc Schermerhorn6, Karen Woo2.
1University of Missouri, Columbia, MO, USA, 2UCLA, Los Angeles, CA, USA, 3Society for Vascular Surgery, Chicago, IL, USA, 4University of Alabama, Birmingham, AL, USA, 5UCSF, San Francisco, CA, USA, 6Beth Israel Deaconess Medical Center, Boston, MA, USA.
Objective: Treatment of claudication is elective, thus good outcomes are imperative. The objective of this study is to examine patterns of claudication management and outcomes after peripheral vascular intervention (PVI) for claudication in the Vascular Quality Initiative (VQI). Methods: Patients undergoing PVI for claudication between 2003-2017 with adequate follow up data were included. Primary outcomes were recurrence(ClaudRecur) and repeat procedures(ReProc). Logistic regression and cox proportional hazards were utilized. For the proportion of procedures, only centers with >20 procedures and surgeons with >10 procedures in 2016 were included. Results: In 2016, the proportion of PVI procedures performed for claudication varied by region:11.3%-31.8%, by center:0-100%, and by surgeon:0-100%. Pre-operative ankle-brachial index was reported in 77%. 13397 patients met inclusion criteria: mean age 66, 61% male, 27% coronary artery disease, 37% diabetes and 84% hypertension. 45.1% were current smokers, >2 arteries were treated in 14.4%, atherectomy was used in 12.5% and 28.3% were discharged without an antiplatelet (AP) AND a statin. Current smoking was associated with increased odds of ClaudRecur(OR 1.11,95%CI 1.01-1.21). Treatment of >2 arteries was associated with increased odds of ClaudRecur(OR 1.18,95% CI 1.06-1.32), shorter time to ClaudRecur(HR 1.2,95%CI 1.09-1.31), increased odds of ReProc(OR 1.23,95%CI 1.07-1.44) and shorter time to ReProc(HR 1.26,95%CI 1.1-1.45). Use of atherectomy was associated with shorter time to ClaudRecur(HR 1.2,95%CI 1.09-1.3), increased odds of ReProc(OR 1.27,95%CI1.08-1.48) and shorter time to ReProc(HR 1.31,95%CI 1.13-1.52). Discharge on AP AND statin was associated with decreased odds of ClaudRecur(OR 0.85,95%CI 0.78-0.93), longer time to ClaudRecur(HR 0.84,95%CI 0.78-0.91), decreased odds of ReProc(OR 0.8,95%CI 0.71-0.9) and longer time to ReProc(HR 0.78,95%CI 0.69-0.87). On life-table analysis, at two years, 32% of patients were free from ClaudRecur and 76% were free from ReProc(Figure). Conclusion: Lack of optimal medical management, use of atherectomy and treatment of >2 arteries are associated with worse outcomes after PVI for claudication. Given that Society for Vascular Surgery guidelines set a benchmark for the outcome of invasive treatment for claudication at a minimum of 50% likelihood of clinical efficacy for two years, these results are concerning and warrant further investigation into factors that influence claudication recurrence after PVI. 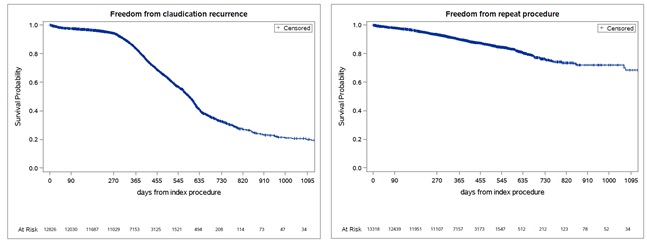
Back to 2019 Abstracts
