Open versus Endovascular repair of Type-IV Thoracoabdominal Aortic Aneurysms
Andelrahman Sherif Saeed Shaaban1, Satinderjit Locham, MD2, Hanaa Dakour-Aridi, MD2, Mahmoud Malas, MD2
1Johns Hopkins University School of Medicine, Baltimore, MD, USA, 2University of California San Diego, La Jolla, CA
OBJECTIVES: Type-IV Thoraco-abdominal aortic aneurysms (TAAA IV) are commonly managed via open surgical repair (OSR). The development of endovascular option with snorkel, branched and fenestrated endografts (EVAR) has provided a minimally invasive alternative to OSR. Very few studies are available in the literature specifically on TAAA IV and are limited to either case series or single institution. Thus, the aim of this study is to use a large national surgical database to evaluate adverse outcomes after OSR vs EVAR of TAAA IV.
METHODS: All patients undergoing repair of TAAA IV were included using the National Surgical Quality Initiative Program (NSQIP) - vascular targeted database (2011-2016). Categorical and continuous variables were analyzed using chi-square, fishers exact and studentís t-test as appropriate. Logistic regression analyses were performed to evaluate primary (mortality) and secondary (acute renal injury, cardiopulmonary failure) outcomes.
RESULTS: A total of 158 patients with Type-IV TAAA were identified. Of which majority of them underwent OSR (62%). Patientsí demographics and comorbidities were similar between the two groups. Except for preoperative renal failure/dialysis which was more common in patients undergoing endovascular repair (12% vs. 3%, P=0.04). Patients in the OSR group required transfusions more frequently (71% vs. 35% P<0.001) and had longer hospital stay (Median [IQR]: 10[7-19] vs. 5[2-10] days; P=0.005). In univariate analysis, no significant difference was seen in 30-day mortality (19% vs. 13%, P=0.39). However, acute renal and cardiopulmonary failures were higher among patients undergoing OSR (figure). After adjusting for potential confounders, 30-day mortality remained not different between the two groups (OR [95%CI]: 1.56[0.64-3.83], P=0.33). Additionally, OSR was associated with almost 6 and 3 folds increase in the odds of renal (OR [95%CI]: 5.60[1.47-21.31], P=0.01) and cardiopulmonary failure (OR [95%CI]: 2.98[1.23-7.23], P=0.02), respectively.
CONCLUSIONS: Using a large nationally representative vascular dataset, our study found no difference in operative mortality between OSR and EVAR of TAAA IV. However, patients undergoing OSR required more transfusion and had significantly higher cardiopulmonary and renal failure and longer length of stay compared to EVAR. Larger prospective studies are needed to compare the durability and cost-effectiveness of the newer endovascular techniques. 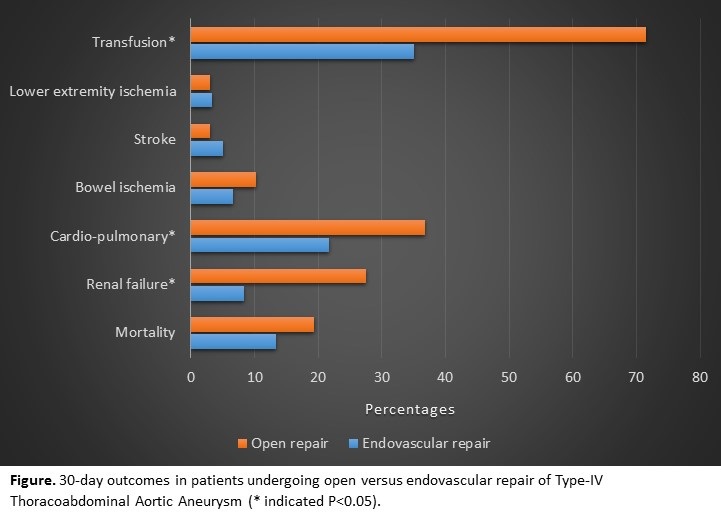
Back to 2019 ePosters
