The Effect of Surgeon Volume on Outcomes Following Carotid Artery Stenting
Chun Li, MD, Chloe A. Powell, MD, Yoel Solomon, BS, Nicholas J. Swerdlow, MD, Patric Liang, MD, Livia E.V.M. De Guerre, MD, Rens R.B. Varkevisser, BS, Kirsten Dansey, MD, Alexander B. Pothof, MD, PhD, Douglas W. Jones, MD, Lars Stangenberg, MD, Marc L. Schermerhorn, MD
Beth Israel Deaconess Medical Center, Boston, MA
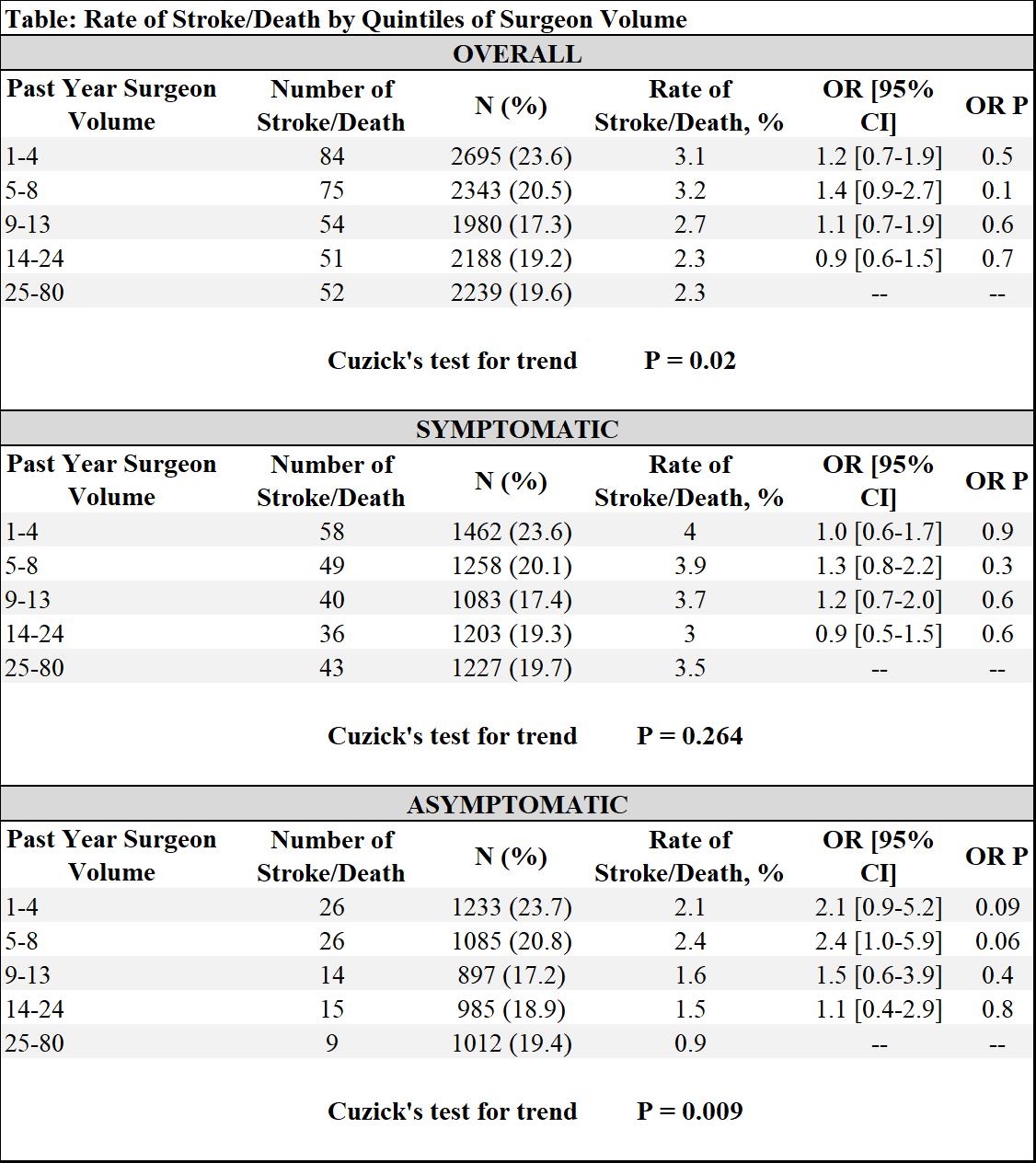
Objective: Effects of surgeon volume on outcomes following carotid endarterectomy (CEA) has been well studied, but impact of surgeon volume on carotid artery stenting (CAS) is poorly characterized. Therefore, we analyzed the effect of surgeon volume on outcomes following CAS in the real-world setting of the Vascular Quality Initiative (VQI) database. Methods: We reviewed patients undergoing CAS within the VQI between 2006-2018 and excluded all patients with missing symptom status, ipsilateral occlusions or emergent cases. We calculated surgeon volume as the total number of cases performed during the 12 months prior to surgery and divided volume into quintiles, grouping into low (lowest quintile), medium (quintile 2-4), or high volume (highest quintile). We assessed for primary outcome of in-hospital stroke/death, as well as other secondary postoperative outcomes, stratified by preoperative symptom. To test for trend among the quintiles, we used non-parametric Cuzick’s test. We also used hierarchical mixed-effects logistic regression with clustering by center and surgeon to adjust for baseline differences. Results: After exclusions, 11,505 patients undergoing CAS were identified, of which 54% symptomatic and 46% asymptomatic, performed by 667 physicians in 214 centers. Calculation of volume in quantiles resulted in the following categories: low (1-4), medium (5-24), high (35-80). Unadjusted rates for stroke/death, stroke, death, cranial nerve injury, myocardial infarction, length of stay >2 days showed no statistically significant differences between volume categories for symptomatic patients. Whereas for asymptomatic patients, there was a trend towards lower rates of stroke/death (low-2.1% vs. med-1.9% vs. high-0.9%, P=.06) and stroke (1.5% vs. 1.2% vs. 0.5%, P=.06, respectively) for higher volumes. Further comparison of stroke/death rates sorted by increasing volume quintile confirms this trend holds true for asymptomatic patients, with a Cuzick trend test P=.009. However, adjusted odds ratios for stroke/death, with the highest quintile as referent, were not significant for any cohort (Table). Conclusion: Surgeons performing greater volumes of carotid revascularizations appear to have lower rates of stroke/death, although the differences are not statistically significant. This trend suggests that CAS should be performed by surgeons with at least medium-high volumes, although the exact relationship between surgeon volume and CAS outcomes warrants further investigation.
Back to 2019 ePosters
