Comparison of Autologous Great Saphenous Vein and Bovine Carotid Artery Graft as a Bypass Conduit in Arterial Trauma
Brendon Reilly, MD, Raphael Blochle, MD, Linda Harris, MD, Hasan Dosluoglu, MD, Mollie O'brien-Irr, NP, James Lukan, MD, Maciej Dryjski, MD PhD, Sikandar Khan, MD
University at Buffalo, Buffalo, NY
Objective: Surgical revascularization remains the mainstay in treating most traumatic arterial injuries, and autologous great saphenous vein (GSV) is the conduit of choice. In trauma, the use of GSV may be limited, and there is little data to guide management in this setting. We have been using bovine carotid artery graft (BCAG, Artegraft), an off the shelf biologic graft, when an expeditious revascularization is required or when available vein is of inadequate caliber. The objective was to review and compare our experience with GSV and BCAG in traumatic arterial injuries requiring bypass or interposition graft. Methods: This is a retrospective review of all patients with a traumatic arterial injury repaired with GSV or BCAG at a single center between April 2014 and October 2016. Outcomes of interest included the presence of wound or graft infection, graft patency, functional status, ambulatory status, and overall limb salvage. Results: Thirty procedures; 17 (57%) lower extremity (LE), 13 (43%) upper extremity (UE) were completed; 12 (40%) BCAG, 18 (60%), autologous vein (AV). Subjects were predominantly male 27 (90%). Mean age 31+ 15 was similar for graft type and injury location. Time to OR and operative time did not vary by injury location or graft type. Hospital length of stay 15+ 12 days was similar for graft type (P= 0.10) and revascularization level (P=0.16). There were no significant differences in ambulatory status at discharge by graft type. Mean follow-up was 19 + 13 months; survival was 100%. Primary patency (PP), secondary patency (SP) and limb salvage (LS) were similar for revascularization level and graft type. Among LE revascularizations, PP (50% vs. 71%; P=0.40), SP (75% vs. 100%; P= 0.23) and LS (80% vs. 86%; P=0.76) was comparable for BCAG and AV. There were no early or late graft infections with either conduit.Conclusions: BCAG appears to be a viable alternative to GSV for revascularization in arterial trauma with comparable primary patency, secondary patency and limb salvage, and low rates of graft related complications. 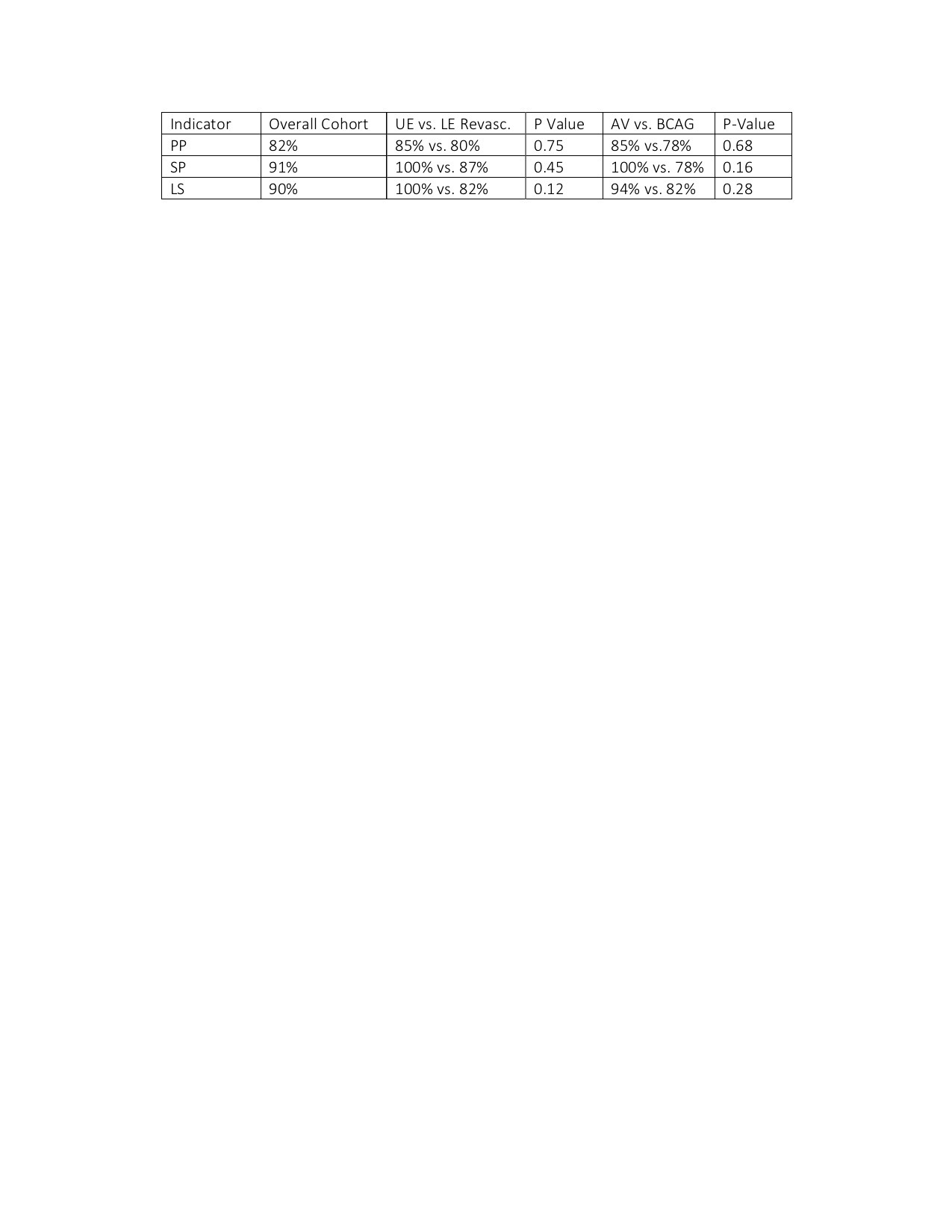
Back to 2019 ePosters
