National Trends in the Treatment of Lower Extremity Arterial Aneurysms: National Disparities in the Era of Endovascular Repair
Nallely Saldana-Ruiz, MD, MPH, Steven Cen, PhD, Anastasia Plotkin, MD, Vincent L. Rowe, MD
University of Southern California, Los Angeles, CA
Objective: Lower extremity arterial aneurysms (LEA), largely of femoral and popliteal origin, are rare and most often found in men. LEA treatment aims to reduce complications of limb-threatening ischemia from embolization and rupture. With advancements in vascular surgery, LEA are now treated with both, open or endovascular approaches. We describe trends in LEA repair over time, as they relate to sex, geographical region, and hospital size.
Methods: The Healthcare Cost and Utilization Project National Inpatient Sample (HCUP-NIS) database between 2000-2012 was queried for a primary diagnosis of LEA (ICD-9CM code 442.3), and LEA repair (ICD-9CM codes 38.38, 38.48, 38.88, 39.79). Survey weights were incorporated following HCUP analysis guideline to obtain population estimates. Temporal trends in LEA and treatment uptake were reported by sex (Male/Female), U.S. region (Northeast/South/Midwest/West) and Hospital size. Rates are reported as per 100 inpatient LEA admissions.
Results: Total inpatient admissions for LEA for males (2000: 4699±225, 2012: 3865±159), were higher than females (2000: 1292±102, 2012: 810±68) per year(Figure). Rates of endovascular therapy LEA repair steadily increased for genders (male from 0.2%±0.1% at 2000 to 12.8%±1.3% at 2012, female from 0% at 2000 to 6.2%±1.9% at 2012), while open surgery decreased (male from 39.9%±1.6% at 2000 to 32.5%±1.6% at 2012, female from 28.8%±2.8% at 2000 to 24.1%±3.4% at 2012). Women demonstrate lower rates of endovascular therapy uptake. While all hospital sizes experienced increased use of endovascular therapy, women had lower rates of endovascular utilization, more starkly at medium than large size hospitals, compared to men. Women also had a lower rate of change in endovascular utilization uptake from 2000-2012 (men 0.00052, women 0.00018 rate of change per year, respectively).
Conclusion: While trends the in use of endovascular intervention for the treatment of LEA have increased over time, clear disparities for women, the U.S. South and Midwest, small hospitals and rural locations persisted. Notably, women showed lower rates of endovascular uptake for the treatment of LEA. Subsequent research efforts should be aimed at understanding the underlying mechanisms driving utilization disparities. 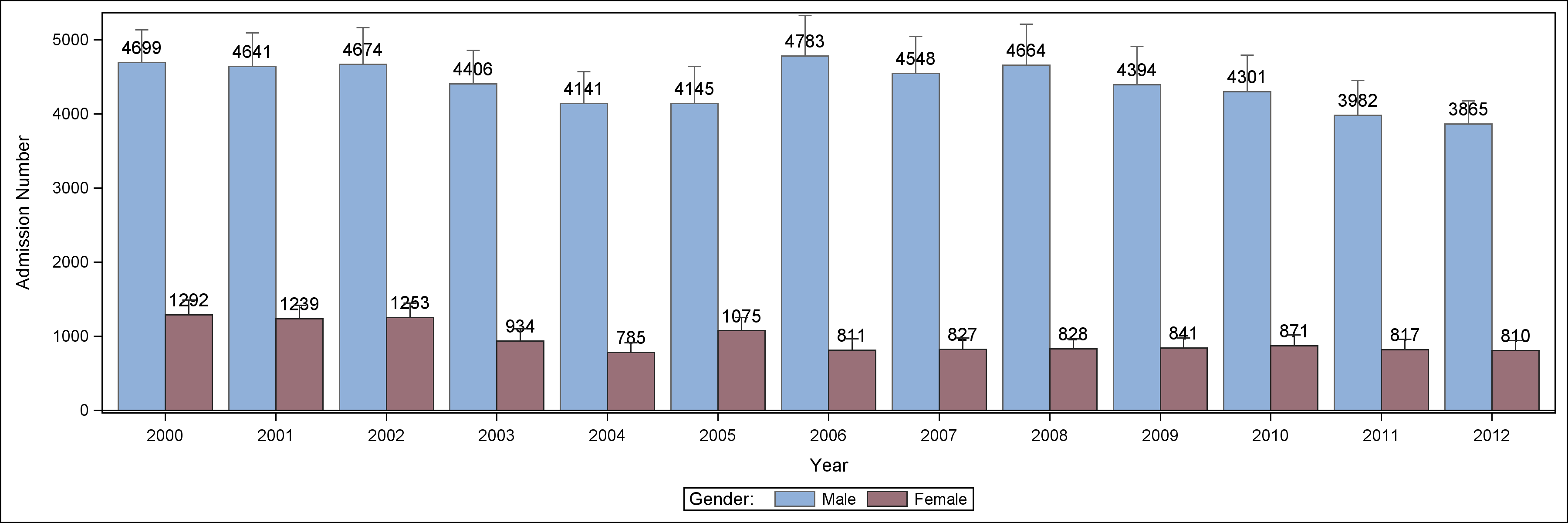
Back to 2019 ePosters
